Scroll to:
Panic Attacks in Patients with Supraventricular Tachycardia: Problems of Differential Diagnosis and Impact on Quality of Life
https://doi.org/10.20996/1819-6446-2021-12-09
Abstract
Aim. To study the psychosomatic relationships and quality of life (QOL) of patients with paroxysmal supraventricular tachycardia (SVT) depending on the presence or absence of panic attacks (PA) in comparison with patients with heartbeat against the background of somatoform autonomic dysfunction.
Material and methods. The study included patients with SVT and heart attacks due to sinus tachycardia in the context of somatoform autonomic disorder (SAD). All patients were interviewed to identify anxiety and depressive disorders (Hospital Anxiety and Depression Scale [HADS] and Hamilton's Depression Scale), QOL assessment (SF-36 questionnaire), and they were also consulted by a psychiatrist who established the presence or absence of PA. According to a visual analogue scale, in points from 0 to 6, we assessed the general state of our patients' health (0 points corresponded to complete health, and 6 points corresponded to a serious illness) and the effect of heartbeat on well-being (0 points - no arrhythmia, 6 points - arrhythmia «nterferes with life»).
Results. The study included 96 patients: 60 with SVT (21 men, 39 women, average age was 51 [33; 61] years) and 36 with heart attacks caused by sinus tachycardia in the framework of somatoform autonomic disorder (10 men, 26 women, average age was 33 [27; 41] years). Panic disorder was diagnosed in the SVT group in 17 patients, accounting for 28.3%. Only 7 patients (41%) could clearly differentiate between SVT and PA attacks. The low sensitivity of the HADS questionnaire in patients with SVT determined the need to consult a psychiatrist for the diagnosis of panic disorders.
Conclusion. PA is typical for 28.3% of patients with SVT. The combination of SVT with PA reduces the QOL of patients due to its mental components, including due to the more frequent occurrence of depressive symptoms. Patients with SAD subjectively perceive the heartbeat as a more significant factor affecting health, compared with patients with SVT. Difficulties in the differential diagnosis of PA and SVT paroxysms in real clinical practice often lead to the appointment of the same therapy without taking into account the differences in the genesis of heartbeats.
Keywords
For citations:
Tsaregorodtsev D.A., Shelukha P.A., Romasenko L.V., Beraya M.M., Sokolov A.V. Panic Attacks in Patients with Supraventricular Tachycardia: Problems of Differential Diagnosis and Impact on Quality of Life. Rational Pharmacotherapy in Cardiology. 2021;17(6):860-866. https://doi.org/10.20996/1819-6446-2021-12-09
Introduction
Heartbeat are one of the most common complaints [1][2], the frequency of which in cardiac patients is up to 40% [3]. Of particular importance is the heartbeat, which occurs paroxysmal. This symptom is caused by cardiac arrhythmias in 38 81% of cases [4][5], among which paroxysmal supraventricular tachycardias (SVT) prevail in the absence of structural heart disease, especially in young patients [6]. But in this cohort, the proportion of heartbeats with a psychogenic nature (31%) is practically comparable to the frequency of cardiac arrhythmias (43%) [5] and is significantly higher than in older patients (4.7%) [4]. Therefore, if a young patient without structural heart disease goes to a polyclinic, and if he complains of paroxysmal heartbeat, the doctor, as a rule, is faced with the task of differential diagnosis of cardiac arrhythmias and sinus tachycardia caused by somatoform autonomic dysfunction, most often within the framework of the panic attack (PA) symptom complex [7].
PA – an attack of anxiety and fear, accompanied by various somatovegetative symptoms. If recurrent PAs are not limited to any special situation or complex of circumstances and, therefore, they are unpredictable, then this is a panic disorder, which according to ICD-10 refers to anxiety-phobic states [8]. We note that it's the heartbeat that is most often detected in patients with PA of all somatic complaints: in 68% of patients with a history of less than 1 year and up to 90% of cases with a longer course of panic disorder [8]. PA is related to SVT paroxysm with a sudden onset of an attack, a rhythmic heartbeat, a possible combination with shortness of breath, chest discomfort, and dizziness [9]. The presence of anxiety, which is the PA essence, is also quite natural for the SVT paroxysm [10]. At the same time, somatoform symptoms in PA (in particular, heartbeat) may prevail over feelings of anxiety and fear. Thus, when tachycardia at the time of a heartbeat attack is not registered on an electrocardiogram (ECG), the differential diagnosis of SVT and PA attacks, based only on a clinical picture assessment, can be difficult. According to the literature, up to 54% of cases of undocumented SVT were initially regarded as PA [7], and vice versa, we assume that up to 20% of PA can be considered by doctors as SVT paroxysms [10]. The high error rate is easily explained by the prevalence of PA in the population - up to 13.2% of people during their lifetime [11], which exceeds the prevalence of SVT (2.25 per 1,000 people) [13]. Therefore, of particular interest may be patients in whom SVT and PA attacks are combined and can occur not only simultaneously («vegetative coloration» of SVT paroxysm), but also independently of each other. Data on the frequency and significance of such a combination are scarce and contradictory [1][7].
The study aim was to study the psychosomatic relationships and quality of life (QoL) in patients with paroxysmal SVT depending on the presence or absence of PA in comparison with patients without somatic pathology with heartbeat against the background of somatoform autonomic dysfunction (within the framework of other psychopathological disorders).
Materials and methods
The study, approved by the local ethics committee, included patients who submitted complaints of heartbeat attack in the period from 2018 to 2020 at the University Clinical Hospital No. 1 (Sechenov University), and signed voluntary informed consent. The exclusion criteria were the presence of structural heart disease (coronary heart disease, congenital and acquired heart defects, left ventricular hypertrophy of any genesis, cardiomyopathy, infiltrative heart disease), the presence of implantable antiarrhythmic devices, canalopathy, age <18 years, pregnancy, breastfeeding, the presence of significant concomitant diseases affecting QoL (oncological diseases, diabetes mellitus, autoimmune diseases, lung diseases occurring with broncho-obstructive syndrome or respiratory failure, liver and kidney disease), any form of atrial fibrillation or atrial flutter, paroxysms of ventricular tachycardia, frequent supraventricular or ventricular premature beats, anemia (hemoglobin level <120 g/l), thyrotoxicosis, patient refusal to participate in the study.
The study included 96 patients (31 men and 65 women). The diagnosis of SVT was made on the basis of an ECG recorded at the time of paroxysm or during a transesophageal electrophysiological study (EPS), and was verified during an intracardiac EPS. The diagnosis of sinus tachycardia in the framework of somatoform autonomic disorder (SAD) was verified using an ECG recorded at the time of heartbeat (including Holter ECG monitoring), as well as in the absence of induction of any other rhythm disturbances during transesophageal EPS. All patients were interviewed to identify anxiety and depressive disorders (Hospital Anxiety and Depression Scale (HADS), Hamilton's Depression Scale) and QoL assessment using the Russian version of the SF-36 questionnaire [12], and they were also consulted by a psychiatrist who established the presence or no history of PA. When assessing QoL, we calculated scores on the scales of physical functioning (PF), role activity (RA), bodily pain (P), general health (GH), vitality (V), social functioning (SF), emotional state (ES) and mental health (MH), the total indicator of physical health (PHtotal) (according to the first four scales) and the total indicator of mental health (MHtotal) (according to the scales from 4 to 8), as well as the average indicator of quality of life (QoLav). When we used the HADS questionnaire, a score of 8-10 on one of the scales indicated subclinical anxiety or depression, 11 scores and above indicated clinically significant anxiety or depression. The Hamilton's Depression Scale was completed during the clinical interview. The total score was determined according to the first 17 points (9 of which were scored from 0 to 4, and 8 were scored from 0 to 2). A total score of 8 to 13 was interpreted as mild depressive disorder, 14 to 18 – moderate depressive disorder, 19 to 22 – severe depressive disorder, more than 23 – extremely severe depressive disorder. In addition, we have developed a visual analogue scale for the subjective assessment of general health and the effect of heartbeat on their well-being. All patients were asked to evaluate in scores from 0 to 6 their general state of health and the effect of heartbeat on well-being: in the first scale, 0 scores corresponded to complete health, and 6 corresponded to a serious illness. In the second scale, 0 scores meant that the arrhythmia was not felt, and 6 scores meant that the arrhythmia «prevents them from living».
Statistical processing of the results was carried out using the SPSS software version 23.0. Data are presented as median (Me) and interquartile range [25%; 75%] or % of the total number of patients. The statistical significance of the differences was assessed using nonparametric methods: Mann-Whitney's, Wilcoxon's, χ2 tests. The probability p<0.05 was considered sufficient to conclude that the differences between the variation series were significant. The difference between the values was regarded as having a tendency towards statistical differences at p>0.05 but <0.1.
Results
Paroxysmal SVT was diagnosed in 60 (21 men, 39 women, average age was 51 [ 33; 61] years) of the patients included in the study (n=96): paroxysmal atrioventricular nodal reciprocal tachycardia was diagnosed in 38 (63.3%) patients, 21 (35%) patients were diagnosed with orthodromic tachycardia, 1 (1.7%) patient was diagnosed with paroxysmal atrial tachycardia. The duration of the anamnesis averaged 9.5 [ 4; 20] years, the frequency of attacks was 1.3 [ 0.3; 4.0] per month, the average heart rate at the time of paroxysm was 170 [ 155; 199] beats per minute. 36 patients (10 men, 26 women, average age was 33 [ 27; 41] years) with no somatic diseases had a heartbeat attack due to sinus tachycardia within the SAD, comorbid to other psychopathological syndromes. Patients in the SAD group were comparable by gender to SVT patients (p=0.308) but were significantly younger (p<0.001).
Panic disorder was diagnosed in the SVT group in 17 patients, accounting for 28.3%. PA, as a rule, in addition to a rapid heart rate, proceeded with a feeling of lack of air, tremors, general weakness, increased sweating, and
avoidance behavior. Only 7 out of 17 patients (41%) could clearly differentiate between SVT and PA attacks. The groups of patients with the presence and absence of PA were comparable in terms of gender, but the patients with PA were somewhat younger (p=0.082) (Table 1). The main characteristics of SVT attacks in the groups with PA and without PA didn't differ significantly: the frequency of attacks per month was 3 [ 0.3; 6] and 1 [ 0.3; 4] (p=0.541), the heart rate at the time of paroxysm was 160 [ 152; 198] and 170 [ 160; 200] (p=0.560), the duration of arrhythmic anamnesis was 14 [ 5.5; 24.5] and 9 [ 3; 20] (p=0.470), time to SVT diagnosis was 6 [ 0.5; 24.5] and 5 [ 2; 19] (p=0.987), the method of stopping paroxysm was determined independently (65% versus 35%) or with medical assistance (40% versus 60%; p=0.070). Also, the patients' assessments of their health in general and the effect of arrhythmias on it turned out to be comparable (see Table 1).
Table 1. Demographic indicators and results of questioning the patients of the studied groups
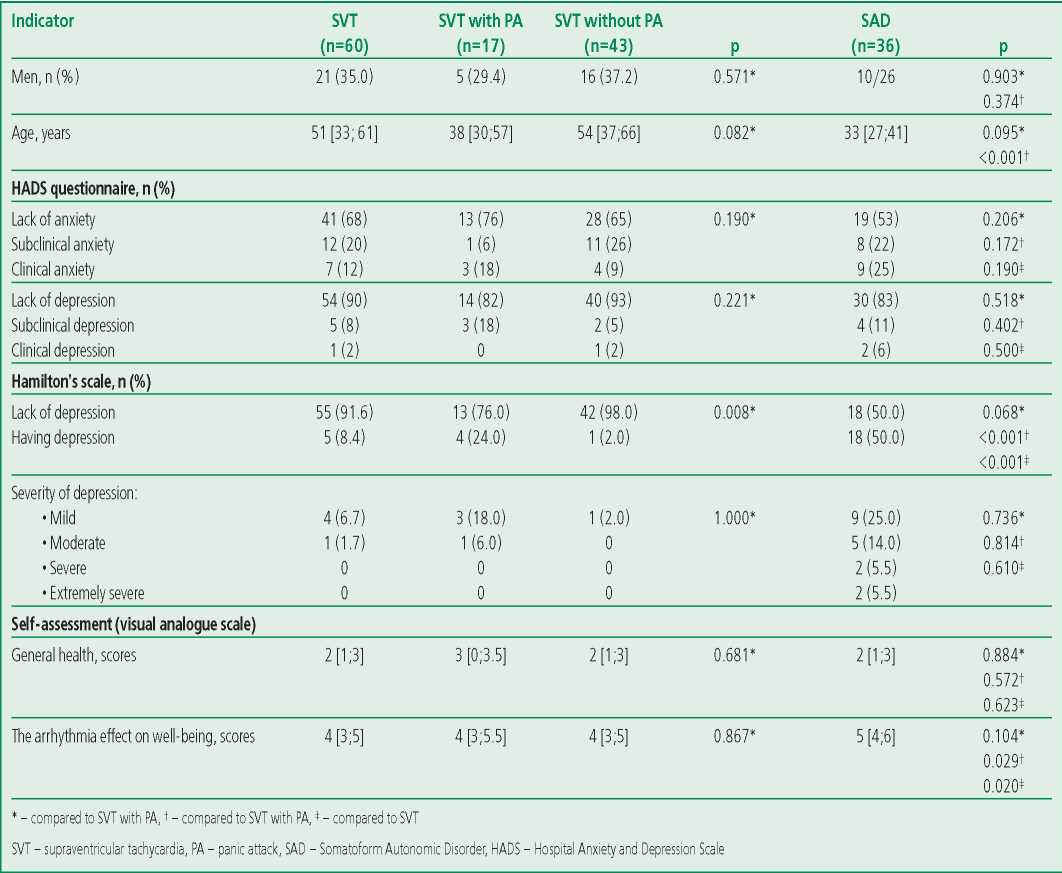
The use of the HADS questionnaire in patients with SVT didn't reveal significant differences in the frequency of anxiety and depressive disorders with or without a history of PA. But a survey of patients by a doctor using the Hamilton's scale showed signs of depression in 24% of patients in the group with PA and only in 2% of patients in the group without PA (p=0.008). The results of the questionnaires were comparable in the case of clinically significant depression according to the HADS data, but the use of the Hamilton's scale allowed us to additionally identify 4 cases of depression, 2 of which were defined by the HADS questionnaire as subclinical, and 2 cases were not recognized. The total coincidence of the results of the patients’ questionnaire survey and the survey by the doctor in diagnosing depression was 38% (see Table 1).
Average QoL was significantly worse in patients with a combination of SVT and PA (p=0.04), which was explained by a decrease in the physical and mental components of QoL compared with patients without PA (Table 2). Thus, the physical condition of patients with PA to a greater extent limited the performance of their daily duties, and such patients had reduced vital activity, felt more «tired», experienced fewer positive emotions, were more often characterized by anxiety and depressive experiences compared with patients with SVT without PA. Comparison of patients with SVT and SAD showed that the feeling of rapid heartbeat associated with sinus tachycardia, with a similar self-assessment of health in general, was subjectively worse tolerated by patients with SAD and was perceived as a more significant factor affecting well-being, compared with paroxysms of true rhythm disturbances in patients with SVT (see Table 1).
Based on the results of collecting anamnesis and analyzing medical records, we compared the treatment of patients with SVT and SAD before they were included in the study. There were no significant differences in the frequency of prescribing drugs with antiarrhythmic activity (p=0.236): beta-blockers were received by 28.3% and 30.6% of patients, respectively, calcium channel blockers were received by 6.7% and 8.3% of patients, antiarrhythmic Class IC drugs were received by 11.7% and 2.8% of patients from the number of patients in the group. The frequency of prescribing psychotropic therapy in the SAD group was 4.2 times less than the rhythm of the accelerating/antiarrhythmic therapy (p <0.001). Only 5 patients (14%) in the SAD group received psychotropic therapy before they were included in the study. The duration of the anamnesis of these five patients was significantly longer than in patients who received only rhythmreducing therapy or didn’t take any drugs (3.0 [ 1.5-22.5] versus 0.5 [ 0.25; 2] years; p=0.008). In the SVT group, 5 patients (8%) also received psychotropic therapy for PA, which didn’t differ significantly from the SAD group (p=0.389).
Subjectively, patients with SVT were more limited in exercise performance (PF score) than patients with SAD (p=0.037; see Table 2), which could be explained by differences in the average age of the groups in addition to the presence of tachycardia paroxysms. But QoLav was significantly worse (p<0.001) in patients with SAD due to a decrease in mental components on the V (p=0.047) and MH (p=0.033) scales, a tendency towards a decrease in SF (p=0.053), ES (p=0.071), which ultimately resulted in a statistically significant decrease in MHtotal (p<0.001) (see Table 2). This fact can be explained by the higher frequency of patients with depressive symptoms and severe depression according to the Hamilton’s questionnaire in the SAD group. At the same time, the use of the HADS questionnaire allowed us to diagnose clinically significant depression 8 times less frequently (see Table 1). The frequency of anxiety detection in the SAD and SVT groups didn’t differ significantly, as well as the frequency of PA in history (44.4% versus 28.3%, respectively; p=0.108).
Table 2. Indicators of quality of life (SF-36) in the studied groups
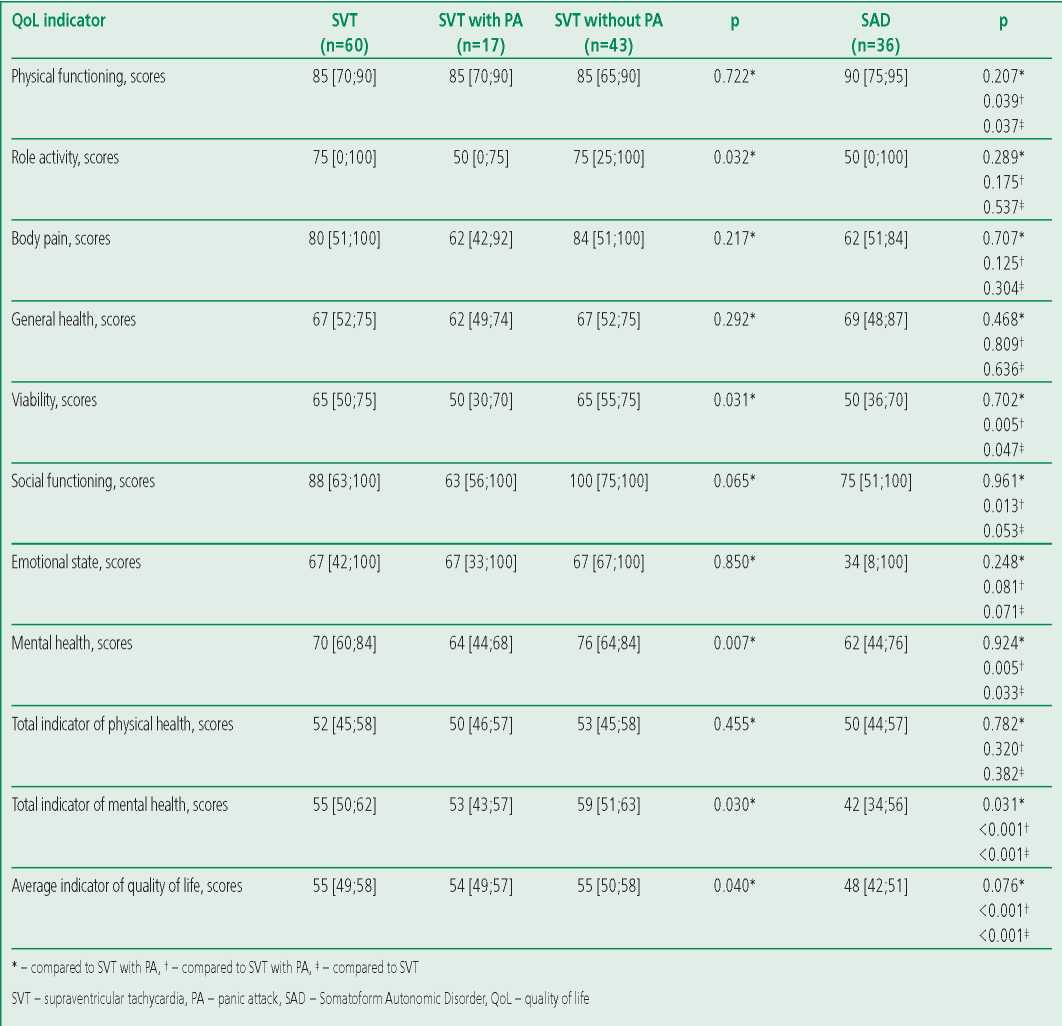
Patients with SVT and PA in anamnesis were comparable to patients with SAD in terms of gender, age, frequency of anxiety disorders, self-assessment of the arrhythmia effect on well-being, and most indicators of the physical and mental component of QoL. Only MHtotal was significantly worse in the SAD group (p=0.031), which caused a trend towards lower QoLav in this group (p=0.076; see Table 2). This fact can be explained by the trend towards a higher frequency of depressive disorders in the SAD group (p=0.068), as well as by the presence of patients with severe forms of depression.
At the same time, patients with SVT without PA were significantly older than patients with SAD (p<0.001) and had a lower PF (=0.039) but all QoL indicators associated with MH in patients with SVT without PA were significantly higher (see Table 2), and the self-assessment of the arrhythmia effect on well-being was significantly lower (see Table 1) than in patients with SAD. The frequency of depression diagnosed using the Hamilton’s questionnaire differed significantly (50% in the SAD group versus 2% in the SVT group without PA; p<0.001), while there were no significant differences in the frequency of anxiety detection in these groups of patients.
Discussion
The relevance of the differential diagnosis of SVT and PA, as well as the complexity of timely diagnosis when combined, are stated by most authors [9][13], but descriptions of individual clinical observations prevail in the literature [9][11], and original studies are rare [1][7]. At the same time, the frequency of detection of PA in patients with SVT depended on the diagnostic method used by the authors. For example, internist doctors in the classic study by T.J. Lessmeier et al. diagnosed panic disorder retrospectively according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [14]. Criteria for panic disorder were identified in 67% of patients with SVT, which was met with controversy among psychiatrists. In general, the incidence of PA appears to be overestimated in 12.5% of outpatients of cardiac profile against the background of diagnosis of panic disorders in the study by T.J. Lessmeier et al [15]. Similar results could be obtained with formal accounting of symptoms, many of which are common to SVT and PA [9]. According to E. Kitzlerov et al., in whose work the anxiety level in patients with SVT was, on the contrary, unusually low, the opposite problem arises when using questionnaires filled out by the patients themselves [1]. Many symptoms are perceived by patients as an integral part of the physical illness and are not reflected in the answers to questions regarding MH. Therefore, the approach taken by us, combining questioning with a consultation with a psychiatrist, is the most rational, and the frequency of PA in patients with SVT in 28.3% more adequately reflects the true picture. At the same time, the low percentage of diagnostics of clinically significant anxiety when using the HADS questionnaire even in the group with undoubted PA, possibly due to dissimulation, may limit the use of this technique as a screening for anxiety disorders in patients with SVT. The incidence of depression among our patients with SVT was low (about 8%), which is very close to the results obtained by E. Kitzlerova et al. [1]. 80% of depression cases were diagnosed in patients with PA. The presence of PA had a negative effect on the QoL of patients, and this effect was more significant than the features of the SVT itself course. A similar opinion was previously expressed by T. Arentz [9]. Patients with SVT and PA in many of the studied characteristics (most of the QoL indicators, selfassessment of the arrhythmia effect on health) were similar to patients with SAD. We can assume that anxietydepressive disorders in SVT have different origins. In addition to nosogenic mental reactions, where the disease (in this case SVT) acts as a traumatic factor and trigger in the development of mental disorders, we also can't exclude the combination of somatic pathology with an independent mental illness in some patients [16]. Further observation of patients after elimination of arrhythmia using catheter ablation and assessment of their mental status in dynamics will allow us to determine the proportion of such patients among patients with SVT. In a study by T.J. Lessmeier et al., it was 4%; however, some patients didn't undergo surgery but received antiarrhythmic therapy, which may have influenced the results obtained [7]. QoL improvement after successful catheter ablation of SVT has been previously shown in a number of studies but the dynamics of anxiety-depressive disorders and the need for psychotropic therapy after arrhythmia elimination need to be clarified [17]. Another aspect considered in our work is the treatment approaches of outpatient doctors to young patients with complaints of a rapid heart rate. Also, the therapy given to patients with SVT and SAD before hospitalization didn't differ in the frequency of use of antiarrhythmic drugs, or in the frequency of use of psychotropic drugs. Thus, cardiologists and therapists prescribed almost the same symptomatic treatment for a rapid heart rate of a completely different genesis. The high frequency of prescribing beta-blockers in this group of patients, in our opinion, has two explanations. Traditionally, neurocirculatory dystonia (actually a synonym for SAD) was considered in Russian cardiology as a functional disorder of the cardiovascular system, which justified the disease manifestation correction with drugs affecting the autonomic nervous system [18]. On the other hand, patients are far from always referred to a psychiatrist for appropriate treatment, even assuming a psychiatric component of clinical symptoms. Thus, only ECG recording at the moment of a rapid heart rate and/or EPS data can guarantee the choice of an adequate approach in the treatment of such patients.
The limitation of our study is the sample size of patients, as well as differences in the age of patients with SVT and SAD. But if the physical and mental components of QoL decrease with age in the general population [12], then in our study patients with SVT were characterized by higher rates of MH compared with younger patients with SAD. Continuing studies on samples characterized by greater homogeneity will allow us to clarify our conclusions.
Study limitations. The limitation of our study is the sample size of patients, as well as differences in the age of patients with SVT and SAD. Continuing studies on samples characterized by greater homogeneity will allow us to increase the power and clarify the results of this study.
Conclusion
PA is characteristic of 28.3% of patients with SVT. Less than half of these patients differentiate between rapid heart rates in PA and SVT paroxysm. The combination of SVT with PA reduces the QoL of patients due to its mental components, including due to the more frequent occurrence of depressive symptoms. Patients with SAD subjectively perceive the rapid heart rate as a more significant factor influencing health, compared with patients with SVT, and have a lower value of the total indicator of mental health, even compared to patients with a combination of SVT and PA. Difficulties in the differential diagnosis of PA and SVT paroxysms in real clinical practice often lead to the appointment of the same therapy without taking into account the differences in the genesis of heartbeats. Further studies is needed to elucidate the genesis of panic disorders in patients with SVT and to determine the optimal tactics for their correction.
Relationships and Activities. None.
Funding. The study was performed with the support of the Sechenov University
References
1. Kitzlerová E, Anders M, Kautzner J, Dohnalová A. Evaluation of psychopathology in patients with paroxysmal supraventricular tachycardia. Exp Clin Cardiol. 2007;12(1):42-5.
2. Raviele A, Giada F, Bergfeldt L, et al. European Heart Rhythm Association. Management of patients with palpitations: a position paper from the European Heart Rhythm Association. Europace 2011;13(7):920-34. DOI: 10.1093/europace/eur130.
3. Alijaniha F, Noorbala A, Afsharypuor S, et al. Relationship Between Palpitation and Mental Health. Iran Red Crescent Med J. 2016;18(3):e22615. DOI:10.5812/ircmj.22615.
4. Probst MA, Mower WR, Kanzaria HK, et al. Analysis of emergency department visits for palpitations (from the National Hospital Ambulatory Medical Care Survey). Am J Cardiol. 2014;113(10):1685-90. DOI:10.1016/j.amjcard.2014.02.020.
5. Weber BE, Kapoor WN. Evaluation and outcomes of patients with palpitations. Am J Med. 1996;100(2):138-48. DOI:10.1016/s0002-9343(97)89451-x.
6. Barsky AJ, Delamater BA, Clancy SA, et al. Somatized psychiatric disorder presenting as palpitations. Arch Intern Med. 1996;156(10):1102-8.
7. Lessmeier TJ, Gamperling D, Johnson-Liddon V, et al. Unrecognized paroxysmal supraventricular tachycardia. Potential for misdiagnosis as panic disorder. Arch Intern Med. 1997;157(5):537-43.
8. Pogosov AV, Nikolaevskaja AO. Clinical and dynamic features of somatized mental disorders with cardiovascular manifestations in patients of the city polyclinic. Siberian Bulletin of Psychiatry and Narcology. 2017;2(95):67-72 (In Russ.).
9. Frommeyer G, Eckardt L, Breithardt G. Panic attacks and supraventricular tachycardias: the chicken or the egg? Neth Heart J. 2013;21(2):74-7. DOI:10.1007/s12471-012-0350-2.
10. Domschke K, KirchhofP, Zwanzger P, et al. Coincidence of paroxysmal supraventricular tachycardia and panic disorder: two case reports. Ann Gen Psychiatry. 2010;9:13. DOI:10.1186/1744-859X-9-13.
11. de Jonge P, Roest AM, Lim CC, et al. Cross-national epidemiology of panic disorder and panic attacks in the world mental health surveys. Depress Anxiety. 2016;33(12):1155-77. DOI:10.1002/da.22572.
12. Amirdzhanova VN, Goryachev LV, Korshunov NI, et al. Population indicators of the quality of life according to the SF-36 questionnaire (results of the multicenter study of the quality of life "MIRAGE"). Scientific and Practical Rheumatology. 2008;(1):36-48 (In Russ.)
13. Brugada J, Katritsis DG, Arbelo E, et al. ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020;41(5):655-720. DOI:10.1093/eurheartj/ehz467.
14. Ballenger JC. Comorbidity of panic and depression: implications for clinical management. Int Clin Psychopharmacol. 1998;13(l4):13-7. DOI:10.1097/00004850-199804004-00003.
15. Morris A, Baker B, Devins GM, Shapiro CM. Prevalence of panic disorder in cardiac outpatients. Can J Psychiatry. 1997;42(2):185-90. DOI:10.1177/070674379704200209.
16. Kanaeva LS, Tsaregorodtsev DA, Romasenko LV, Mahaeva DV. Systematization of mental disorders in cardiac arrhythmias. Mental Health. 2020;11:62-72 (In Russ.).
17. Walfridsson U, Walfridsson H, Arestedt K, Strömberg A. Impact of radiofrequency ablation on health-related quality of life in patients with paroxysmal supraventricular tachycardia compared with a norm population one year after treatment. Heart Lung. 2011;40(5):405-11. DOI:10.1016/j.hrtl-ng.2010.09.004.
18. Makolkin VI, Abbakumov SA, Sapozhnikov AA. Neurocirculatory dystonia (clinic, diagnosis, treatment). Cheboksary: Chuvashia; 1995 (In Russ.).
About the Authors
D. A. TsaregorodtsevRussian Federation
Dmitrii A. Tsaregorodtsev.
Moscow.
eLibrary SPIN 2840-5301
P. A. Shelukha
Russian Federation
Polina A. Shelukha.
Moscow.
eLibrary SPIN 3424-7156
L. V. Romasenko
Russian Federation
Lubov V. Romasenko.
Moscow.
eLibrary SPIN 6225-4232
M. M. Beraya
Russian Federation
Maka M. Beraya.
Moscow.
eLibrary SPIN 4124-3813
A. V. Sokolov
Russian Federation
Aleksey V. Sokolov.
Moscow.
eLibrary SPIN 8265-4292
Review
For citations:
Tsaregorodtsev D.A., Shelukha P.A., Romasenko L.V., Beraya M.M., Sokolov A.V. Panic Attacks in Patients with Supraventricular Tachycardia: Problems of Differential Diagnosis and Impact on Quality of Life. Rational Pharmacotherapy in Cardiology. 2021;17(6):860-866. https://doi.org/10.20996/1819-6446-2021-12-09
JATS XML
















































