Scroll to:
Challenges of Statin Therapy in Clinical Practice (According to Outpatient Register «PROFILE» Data)
https://doi.org/10.20996/1819-6446-2022-02-02
Abstract
Aim. To identify the main problems of statin therapy in patients with high and very high cardiovascular (CV) risk in real clinical practice.
Material and methods. The general information of the study was based on data from 2,457 patients who were included in the register before November 30, 2020: 1,250 men (50.9%) and 1,207 (49.1%) women. A more detailed analysis was performed for groups of patients with high and very high CV risk who had indications for statin treatment at the time of inclusion in the register: out of 2457 patients, 1166 people had very high CV risk, 395 was at high CV risk (a total of 1561 people, the average age of patients was 64.4±11.0 years).
Results. Information on the parameters of the lipidogram – the level of total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) was available in 1918 (78.1%) and 1546 (62.9%) patients, respectively. Of 1561 patients with high and very high CV risk, TC and LDL-C levels were analyzed in 1221 (78.2%) and 956 (61.2%) cases, statistically significantly more often in patients with high CV risk (p<0.05). Statins were recommended only to 823 (52.7%) patients with high and very high CV risk. Patients with very high CV risk received such appointments 4 times more often than patients with high CV risk: odds ratio (OR) 4.2; 95% confidence interval (CI) 3.2-5.3 (p<0.001). Doctors preferred atorvastatin in prescriptions (n=456, 55.4%), rosuvastatin (n=244, 29.7%) and simvastatin (n=121, 14.7%) were in second and third places. The target level of LDLC was 2 times more often achieved in patients with high CVR, compared with patients with very high CV risk: OR = 2.0, 95% CI 1.4-3.0 (p<0.001).
Conclusion. The main problems of statin treatment in real clinical practice remain the non-assignment of these drugs to patients who have indications for such therapy and the failure to achieve the target levels of lipidogram indicators, which may probably be due to the clinical inertia of doctors regarding titration of statin doses, and in some cases caused by the choice of drugs that are not the most effective in reducing LDL cholesterol. Patients with very high CV risk are 4 times more likely to receive a recommendation to take statins compared to patients with high CV risk, but the target level of LDL cholesterol is reached in them 2 times less often.
For citations:
Martsevich S.Yu., Lukina Yu.V., Kutishenko N.P., Zagrebelnyy A.V., Tolpygina S.N., Voronina V.P., Dmitrieva N.A., Lerman O.V., Nekoshnova E.S., Budaeva I.V., Blagodatskikh S.V., Aslanova B.B. Challenges of Statin Therapy in Clinical Practice (According to Outpatient Register «PROFILE» Data). Rational Pharmacotherapy in Cardiology. 2022;18(1):73-78. https://doi.org/10.20996/1819-6446-2022-02-02
Introduction
Atherosclerotic cardiovascular diseases continue to lead among the main causes of death in the population in most countries of the world [1][2]. The first place among drugs that have a pathogenetic effect on the atherosclerosis process belongs to statins (HMG-CoA reductase inhibitors). These are the most studied lipid-modifying agents that improve the prognosis of the disease and life in patients with atherosclerotic cardiovascular diseases. Statins are recommended for most patients with high and very high risk of cardiovascular complications and are the basis of lipid-lowering therapy in such patients [1][6]. It remains far from optimal despite improvements in statin prescribing and achievement of target cholesterol levels (total cholesterol and low-density lipoprotein cholesterol [LDL-C]) in large trials (EUROASPIRE IV, EUROASPIRE V, ARGO, etc.) [7-9]. Also, researchers note difficulties in finding and implementing a universal strategy for the most effective use of statins in clinical practice [10].
The aim of this study is to determine the features and main problems of statin therapy, as well as to assess the possibility of achieving the target level of lipid profile parameters in the treatment of patients with high and very high cardiovascular risk (CV risk) with drugs from the statin group in clinical practice.
Materials and methods
The study was of the nature of a single-stage cohort study. Data from the outpatient register of patients with cardiovascular diseases and their risk factors «PROFILE» were analyzed to achieve the aim of the study.
The «PROFILE» register is a register of the department of preventive pharmacotherapy of the Federal State Budgetary Institution « National Medical Research Center for Therapy and Preventive Medicine » of the Ministry of Health of Russia, which includes all patients who applied for a consultation about cardiovascular diseases or to assess their possible participation in clinical trials. The initial consultation with a cardiologist is the first visit/inclusion of the patient in the registry. The register database has been formed since 2014.
Analysis of patient data was performed at the time of inclusion in the registry since this information most reflects the state of the statin treatment problem in clinical practice. The target value of LDL-C was the
level of <1.8 mmol/l for patients with very high risk and <2.5 mmol/l for patients with high cardiovascular risk (target values according to clinical guidelines in force during the main period of inclusion of patients in the study [4][11])
The study's general information was based on 2,457 patients (1,250 men [ 50.9%] and 1,207 [ 49.1%] women) who were enrolled up to November 30, 2020. The average age of patients was 61.4±10.5 years. A more detailed analysis was performed for groups of patients with high and very high cardiovascular risk (that is, who had indications for statin treatment) at the time of inclusion of patients in the register.
Statistical data processing was performed using the SPSS 23.0 program (IBM Statistics, USA). The normality of the distribution of quantitative variables was determined using Shapiro-Wilk's test. The variables analyzed in the study were presented as mean values (M) and standard deviations (δ) or median (Me) and interquartile range [ 25%; 75%]. Qualitative variables are presented as absolute and percentage values. Student's t-test and Pearson's chi-square were used for comparative analysis and determination of odds ratio (OR) and 95% confidence intervals (CI) for 2×2 contingency tables. Differences were considered statistically significant at p<0.05.
Results
Information about the analysis of the total cholesterol level at the time of inclusion in the register was available only in 1,918 (78.1%) patients: 948 men (50.6%) and 970 (49.4%) women. The determination of LDL-C was performed in 1,546 patients (62.9%): 753 (48.7%) men and 793 (51.3%) women.
The frequency of appointment of analyzes for total cholesterol was 1 analysis in 15 [ 11; 26 ] months (that is, approximately once a year). The LDL-C level was determined somewhat less frequently - 1 time in 16 [ 11; 27 ] months.
The CV risk was determined in 1,166 (47.5%) of 2,457 patients as very high, and 395 (16.1%) had high CV risk. Thus, 1,561 patients were eligible for statin therapy. The nosological profile of patients with high and very high cardiovascular risk is presented in Table 1. The average age of patients was 64.4±11.0 years. Patients with very high cardiovascular risk were significantly older than patients with high cardiovascular risk (65.7±10.3 versus 60.4±12.3 years; p<0.05).
Table 1. Nosological profile of patients with high and very high cardiovascular risk

At the time of inclusion in the outpatient registry of 1,561 patients with high and very high CV risk, lipid profile parameters (total cholesterol and LDLC) were determined in 1,221 (78.2%) and 956 (61.2%) cases, respectively. Comparative analysis revealed that at the time of inclusion of patients in the register, lipid profile parameters were more often determined in patients with high cardiovascular risk compared to patients with very high cardiovascular risk (Table 2).
Table 2. Availability of lipid profile data at enrollment visit in patients at high and very high CV risk (n=1561)

These drugs were recommended only to 823 (52.7%) patients, despite the presence of indications for the appointment of statins in patients with high and very high CV risk. Patients with very high CV risk received such prescriptions 4 times more often than patients with high CV risk (OR=4.2; 95% CI=3.2- 5.3, p<0.001; Fig. 1).

Figure 1. Prescription of statins to patients with high and very high cardiovascular risk at the time of inclusion in the registry
We also note that doctors preferred atorvastatin in prescriptions (55.4%; n=456); rosuvastatin (29.7%; n=244) and simvastatin (14.7%; n=121) were in second and third place. Pitavastatin and lovastatin were recommended in 2 patients.
Figure 2 provides information on the statin (international nonproprietary name) class of drugs that were prescribed to patients with high and very high CV risk before inclusion in the outpatient «PROFILE» register. The frequency of prescribing different statins in the compared groups didn't differ (p=0.7).
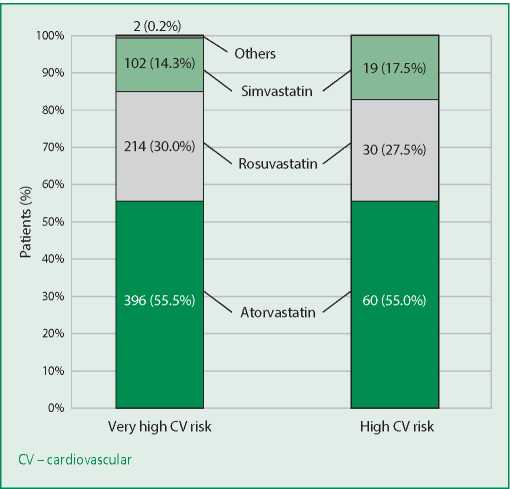
Figure 2. Statins prescribed for patients at high and very high cardiovascular risk at inclusion in the registry
At the time of inclusion in the «PROFILE» registry, lipid profiles were present in 674 (57.8%) of 1,166 patients with very high CV risk and in 282 (71.4%) of 395 patients with high CV risk. We analyzed in what percentage of cases the LDL-C level was <1.8 mmol/l in patients with very high CV risk, and <2.5 mmol/l in patients with high CV risk (Fig. 3).

Figure 3. Frequency of achieving the target level of LDL-C in the compared groups
The frequency of achieving the LDL-C target level was statistically significantly higher in the group of patients with high risk than in patients with very high cardiovascular risk (OR=2.0; 95% CI=1.4-3.0; p<0.001).
Discussion
The statin prescription to patients with high and very high cardiovascular risk has been recognized and reflected in the clinical guidelines (for the treatment of such patients) of many world professional communities [1-6][11-13]. Moreover, this provision of recommendations has the highest class and level of evidence. Nevertheless, the results of many observational or cross-sectional studies demonstrate that the non-prescription of statins when patients have indications for such treatment is one of the most significant problems of statin therapy in clinical practice [9][14-18].
However, there is certainly a positive trend in the dynamics of statin prescriptions for patients with high or very high CV risk over the past 10-15 years. For example, according to a comparative analysis of two hospital registries (Lyubertsy mortality studies), LMS-1 and LMS-3, the frequency of statin prescription to patients with acute coronary syndrome (ACS) at the outpatient stage prior to a coronary event increased from 2.0% to 4.9% from 2005 to 2015, while remaining extremely low. If we accept that ACS could be the onset of CHD, the authors of this comparative analysis estimated the frequency of statin prescription in patients with a history of CHD: only 12.5% of patients received such therapy. At the same time, all of them survived with ACS, and persons taking statins were not among the patients who died [14].
The data obtained in our study, according to which only half of the patients with high and very high CV risk received recommendations for taking statins, are fully consistent with the results of the cross-sectional cohort multicenter study ARGO: statins were not prescribed in 45.2% of 18,273 patients with high and very high CV risk [9]. According to the results of the observational study SANTORINI, in Europe, almost one in five of 9,606 patients with high or very high risk of cardiovascular complications (18.6%) didn't receive lipid-lowering therapy [15].
According to the prospective observational multicenter study PRIORITET, 37.6% of high and very high-risk patients who had no absolute contraindications to statin treatment were not prescribed these drugs in an outpatient setting [16]. Nevertheless, a brief briefing of the attending doctors on the main provisions of the current clinical recommendations, as well as regular monitoring of patients, significantly improved the situation with the statin prescription and the adherence of patients to this treatment [17].
An even more difficult issue in the treatment of patients with high and very high cardiovascular risk with statins is the achievement of target values of lipid profile parameters, mainly, the LDL-C level. The tendency to reduce the target level of this indicator (the maximum possible reduction), which continues in the clinical recommendations of the last decade, especially for patients with very high cardiovascular risk, leads to the fact that it can be achieved in clinical practice in an ever smaller percentage of cases [18][19]. Medical inertia in prescribing highintensity lipid-lowering therapy plays an important role in this.
Of course, an integral part of the problems associated with statin therapy and the effectiveness of this treatment are the issues of patient adherence to the prescribed treatment [17][20], which were not studied in our study. However, we note that the issue of patient adherence is always secondary to physician adherence to clinical guidelines that statin therapy should be initiated in patients with high and very high CV risk, and target levels of lipid profile should be achieved.
According to the results of the analysis, atorvastatin and rosuvastatin, noted in clinical recommendations, as statins with the maximum lipid-lowering efficacy, prevailed in medical prescriptions. However, simvastatin was recommended to one in seven patients in our study.
Study limitations. The PROFILE outpatient registry is prospective, but the study performed is a crosssectional, single-center, and cohort study, the results of which reflect the characteristics of statin treatment in high and very high-risk patients in clinical practice.
Conclusion
The main problems of statin treatment in clinical practice are the non-prescription of these drugs to patients with indications for such therapy and the failure to achieve the target levels of lipid profile parameters, which may be due to the clinical inertia of doctors regarding titration of statin doses, and in some cases, this may be associated with the choice of drugs that are not the most effective in reducing the LDL-C level. Patients with very high CV risk are 4 times more likely to receive a statin recommendation compared to patients with high CV risk, but they reach their target LDL-C level 2 times less often.
Relationships and Activities. None.
Funding. The PROFILE registry is maintained by the National Medical Research Center for Therapy and Preventive Medicine. Unloading of impersonal information of patients (n=2457) from the database of the register "PROFIL" on the nosology of dyslipidemia, necessary for research work and its statistical processing was performed with the sponsorship of EGIS-RUS LLC (Hungary), which did not affect the results in any way , conclusions and own opinion of the authors.
References
1. Visseren FLJ, Mach F, Smulders YM, et al. ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227-337. DOI:10.1093/eurheartj/ehab484.
2. World Health Organization (WHO). Cardiovascular diseases (CVD) [cited 2021 Jul 30]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)#:~:text=Cardiovascular%20diseases%20(CVDs)%20are%20the,%2D%20and%20middle%2Dincome%20countries.
3. Reiter-Brennan C, Osei AD, Iftekhar Uddin SM, et al. ACC/AHA lipid guidelines: Personalized care to prevent cardiovascular disease. Cleve Clin J Med. 2020;87(4):231-9. DOI:10.3949/ccjm.87a.19078.
4. Cardiovascular prevention 2017. National guidelines. Russian Journal of Cardiology. 2018;(6):7-122 (In Russ.) DOI:10.15829/1560-4071-2018-6-7-122.
5. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87. DOI:10.4158/EP171764.APPGL.
6. The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). ESC/EAS guidelines for the management of dyslipidaemia. Eur Heart J. 2020;41(1):11-188. DOI:10.1093/eurheartj/ehz455.
7. Reiner Ž, De Backer G, Fras Z, et al. Lipid lowering drug therapy in patients with coronary heart disease from 24 European countries--Findings from the EUROASPIRE IV survey. Atherosclerosis. 2016;246:243-50. DOI:10.1016/j.atherosclerosis.2016.01.018.
8. Santos RD. EUROASPIRE V and uncontrolled risk factors in primary prevention: Atherosclerotic cardiovascular disease in the making. Eur J Prev Cardiol. 2020 Apr 1:2047487320915662. DOI:10.1177/2047487320915662.
9. Akhmedzhanov NM, Nebieridze DV, Safaryan AS, et al. Analysis of hypercholesterolemia prevalence in the outpatient practice (according to the ARGO study): part I. Rational Pharmacotherapy in Cardiology. 2015;11(3):253-60 (In Russ.) DOI:10.20996/1819-6446-2015-11-3-253-260.
10. Jones LK, Tilberry S, Gregor C, et al. Implementation strategies to improve statin utilization in individuals with hypercholesterolemia: a systematic review and meta-analysis. Implementat Sci. 2021;16(1):40. DOI:10.1186/s13012-021-01108-0.
11. Diagnosis and correction of lipid metabolism disorders for the prevention and treatment of atherosclerosis. Russian guidelines (V revision) [cited 2021 Jul 30]. Available from: https://scardio.ru/content/Guidelines/rek_lipid_2012.pdf (In Russ.)
12. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1046-e1081. DOI:10.1161/CIR.0000000000000624.
13. Kukharchuk VV, Ezhov MV, Sergienko IV, et al. Eurasian Association of Cardiology (EAC)/ Russian National Atherosclerosis Society (RNAS, Russia) guidelines for the diagnosis and correction of dyslipidemia for the prevention and treatment of atherosclerosis (2020). Eurasian Heart Journal. 2020;(2):6-29 (In Russ.) DOI:10.38109/2225-1685-2020-2-6-29.
14. Semenova YV, Zagrebelnyy AV, Kutishenko NP, et al. Assessment of changes in quality of prehospital treatment of patients with acute coronary syndrome in the last few years: LIS-1 vs LIS-3 registries. Rational Pharmacotherapy in Cardiology. 2017;13(6):827-34 (In Russ.) DOI:10.20996/1819-6446-2017-13-6-827-834.
15. Ray KK, Haq I, Bilitou A, et al. Evaluation of contemporary treatment of high-and very high-risk patients for the prevention of cardiovascular events in Europe - Methodology and rationale for the multinational observational SANTORINI study. Atherosclerosis Plus. 2021;43:24-30. DOI:10.1016/j.athplu.2021.08.003.
16. Martsevich SY, Lukina YV, Kutishenko NP, et al. Features and main problems of treating patients with high and very high cardiovascular risk with statins in real clinical practice (according to the data of the “PRIORITET” research). Cardiovascular Therapy and Prevention. 2018;17(6):52-60 (In Russ.) DOI:10.15829/1728-8800-2018-6-52-60.
17. Martsevich SY, Lukina YV, Kutishenko NP, et al. Adherence to Statins Therapy of High and Very High Cardiovascular Risk Patients in Real Clinical Practice: Diagnostics and Possible Ways to Solve the Problem (According to the PRIORITY Observational Study). Rational Pharmacotherapy in Cardiology. 2018;14(6):891-900 (In Russ.) DOI:10.20996/1819-6446-2018-14-6-891-900.
18. Danese MD, Gleeson M, Kutikova L. et al. Management of lipid-lowering therapy in patients with cardiovascular events in the UK: a retrospective cohort study. BMJ Open. 2017;7(5):e013851. DOI:10.1136/bmjopen-2016-013851.
19. Rachamin Y, Meier R, Rosemann T, et al. Statin treatment and LDL target value achievement in Swiss general practice - a retrospective observational study. Swiss Med Wkly. 2020;150:w20244. DOI:10.4414/smw.2020.20244.
20. Spence JD, Dresser GK. Overcoming Challenges With Statin Therapy. J Am Heart Assoc. 2016;27;5(1):e002497. DOI:10.1161/JAHA.115.002497.
About the Authors
S. Yu. MartsevichRussian Federation
Sergey Y. Martsevich.
Moscow.
Yu. V. Lukina
Russian Federation
Yulia V. Lukina.
Moscow.
N. P. Kutishenko
Russian Federation
Natalia P. Kutishenko.
Moscow.
A. V. Zagrebelnyy
Russian Federation
Alexander V. Zagrebelnyy.
Moscow.
S. N. Tolpygina
Russian Federation
Svetlana N. Tolpygina.
Moscow.
V. P. Voronina
Russian Federation
Victoria P. Voronina.
Moscow.
N. A. Dmitrieva
Russian Federation
Nadezhda A. Dmitrieva.
Moscow.
O. V. Lerman
Russian Federation
Olga V. Lerman.
Moscow.
E. S. Nekoshnova
Russian Federation
Elena S. Nekoshnova.
Moscow.
I. V. Budaeva
Russian Federation
Irina V. Budaeva.
Moscow.
S. V. Blagodatskikh
Russian Federation
Svetlana V. Blagodatskikh.
Moscow.
B. B. Aslanova
Russian Federation
Bela B. Aslanova.
Moscow.
Review
For citations:
Martsevich S.Yu., Lukina Yu.V., Kutishenko N.P., Zagrebelnyy A.V., Tolpygina S.N., Voronina V.P., Dmitrieva N.A., Lerman O.V., Nekoshnova E.S., Budaeva I.V., Blagodatskikh S.V., Aslanova B.B. Challenges of Statin Therapy in Clinical Practice (According to Outpatient Register «PROFILE» Data). Rational Pharmacotherapy in Cardiology. 2022;18(1):73-78. https://doi.org/10.20996/1819-6446-2022-02-02
















































