Scroll to:
Risk of Venous Thromboembolic Complications in Patients with Atrial Fibrillation: a Systematic Review and Meta-analysis
https://doi.org/10.20996/1819-6446-2022-06-02
Abstract
Aim: The aim of this meta-analysis and systematic review was to evaluate the possible connection between AF and VTE.
Material and methods. Atrial fibrillation (AF) and atrial flutter (AFL) contribute to intra-atrial blood stasis which leads to thrombus formation with its embolization. There is some evidence that AF can be a risk factor for deep vein thrombosis (DVT) and pulmonary embolism (PE). The following databases were searched: PubMed (MEDLINE), EMBASE, Google Scholar, the Cochrane Central Register of Controlled Trials. The time frame for conducting a systematic literature search ranged from January 1, 1990 to November 1, 2021. The diagnosis of atrial fibrillation had to be confirmed by using ECG. The diagnosis of VTE could be made with Doppler imaging, ventilation/perfusion scan, CT angiography, venography, angiography or autopsy. Only the three studies with 102192 patients meeting the requirement were included in the meta-analysis.
Results. The prevalence of DVT and PE were assessed using incidence rate ratios (IRR) method of the inverse variance random effects model and its 95% confidence interval (CI). The significant association between atrial fibrillation and pulmonary embolism was found (IRR, 4.18 95% Cl 1.958.98). Also there is obvious association between DVT and AF (IRR, 2.97 95% Cl 2.18-4.03).
Conclusion. It can be concluded that the increased risk of developing VTE is associatedwith concomitant AF.
For citations:
Sokolova A.A., Kudriavtseva A.A., Kostokova N.V., Zaikina M.P., Gebekova Z.A., Napalkov D.A., Zolotukhin I.A. Risk of Venous Thromboembolic Complications in Patients with Atrial Fibrillation: a Systematic Review and Meta-analysis. Rational Pharmacotherapy in Cardiology. 2022;18(3):236-241. https://doi.org/10.20996/1819-6446-2022-06-02
Introduction
Currently, atrial fibrillation (AF) is one of the most common cardiac arrhythmias. It affects about 2-4% of the adult population worldwide [1]. It has been proven that atrial fibrillation and atrial flutter contribute to intra-atrial blood stasis which creates conditions for thrombus formation and thrombus embolization [2]. It is also well known that blood clots which can form in the left atrium due to AF can lead to ischemic stroke [3] and myocardial infarction [4].
However, some recent studies showed that thrombus formation can also occur in the right atrium in patients with AF and may cause pulmonary embolism (PE). The frequency of atrial fibrillation in patients with acute PE is 15-21%. While the other studies showed that PE can cause pulmonary hypertension and, as a result, increase pressure in the right chambers of the heart and deformation of the right atrial wall, which, in turn, can cause AF [5-7].
There is also some evidence that AF can be a risk factor for deep vein thrombosis (DVT) which can be explained by poor hemodynamics and abnormal hemostasis such as an increased levels of fibrinogen in the blood serum, D-dimer, von Willebrand factor (vWF), factor VIII: C,β-thromboglobulin (β-TG), fibrinopeptide A, platelet factor 4 (PF4) and thrombin-antithrombin complex III (TAT) [8-10].
Despite the interaction between these events, this issue has not sufficiently been studied yet. There is a possibility that AF and VTE may be the result of different diseases in the same patients rather than the interactions of this conditions. The existing studies [11-14] researching links between AF and VTE have a number of limitations, therefore, it’s impossible to extrapolate results to the entire population. The purpose of our systematic review and meta-analysis is to assess the impact of AF on the development of VTE.
Material and methods
Literature search
The following databases were researched: PubMed (MEDLINE), EMBASE, Google scholar databases, the Cochrane Central Register of Controlled Trials. The time frame for conducting a systematic literature search related to AF and VTE ranged from January 1, 1990 to November 1, 2021 (the date of our final search).
We used such search words with MeSH Terms as (atrial fibrillation or AF) AND (venous thromboembolism or VTE) OR (deep vein thrombosis or DVT) OR (pulmonary embolism or PE).
We also performed a manual search to identify additional studies of interest.
The Guidelines of the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement were used for conducting and reporting the systematic literature review [15].
Study eligibility
Two investigators screened the titles and abstracts of all the articles independently to identify the suitable ones. Then the same people reviewed the full-text copies of selected articles to ensure their eligibility. The arising disagreements and uncertainties were resolved by consensus of all reviewers.
We included the population-based cohort studies published after 2000 in the English language. The diagnosis of atrial fibrillation had to be confirmed by using ECG. The diagnosis of VTE could be made with Doppler imaging, ventilation/perfusion scan, CT angiography, venography, angiography or autopsy. The papers in other languages than English and with insufficient data were excluded. There were no restrictions based on race or geographic location.
Quality Assessment
The methodological quality of the included studies was assessed by using the Newcastle-Ottawa Quality Assessment scale for observational studies [16].
Statistical analysis
The outcomes of VTE both for DVT and PE were assessed using dichotomous data retrieved from the population-based cohort studies. The next stage was to estimate the incidence rate ratio (IRR) using the inverse variance random effects model and its 95% confidence interval (CI).
To determine Statistical heterogeneity a χ2 test and an I2 statistic were calculated.
Significant heterogeneity was considered present at p<0.10 and I2>50%. The meta-analysis was conducted using the Review Manager 5.4.1 software statistical analysis.
The study was not registered with an international prospective register of systematic reviews.
Results
During the initial literature search we scanned 94 papers. Based on the title and the abstract only 42 publications were selected for full-text review. After full-text screening 8 papers were chosen for analysis. The others publications were excluded because of different outcome measurements and inappropriate data for pooled analysis. Of the 8 studies identified, 5 were excluded as there were no appropriate data available for a meta-analysis (Fig. 1). The three studies meeting the requirement were included in Table 1.
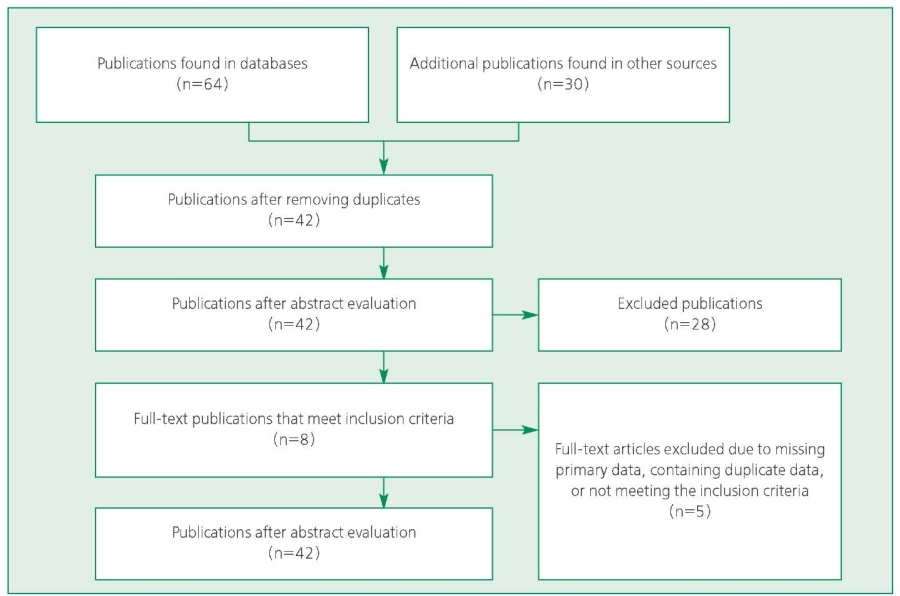
Figure 1. Schema of search results for this meta-analysis
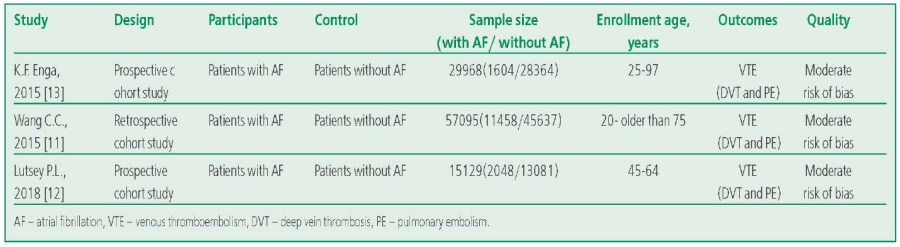
Table 1. Characteristic of studies included in the meta-analysis
121 (0.8%) cases of pulmonary embolism occurred in 15 110 patients with AF compared to the control group. 480 (0.6%) cases of PE were registered in 87 082 patients without AF. The significant association between atrial fibrillation and pulmonary embolism was found (IRR 4.18, 95% CI 1.95-8.98, I2 = 92%; Fig. 2).
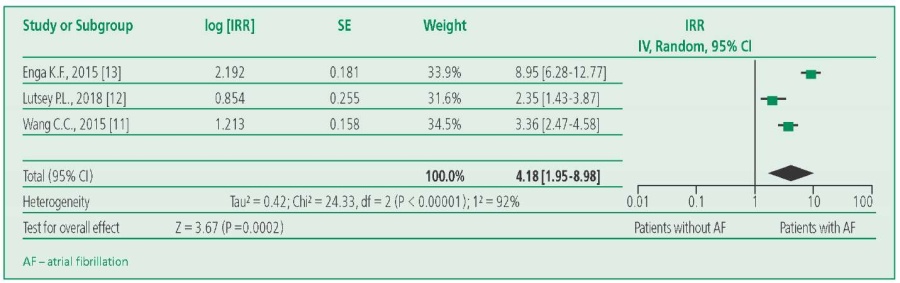
Figure 2. Forest plot of risk ratio (random effects model) results: pulmonary embolism in patients with or without atrial fibrillation
Also, out of 15 110 patients with AF DVT was found in 198 patients (1.3%). Only 1035 (1.2%) cases of DVT were confirmed in the control group (n=87 082). There was obvious association between DVT and AF (IRR 2.97, 95% CI 2.18-4.03, I2=70%; Fig. 3).
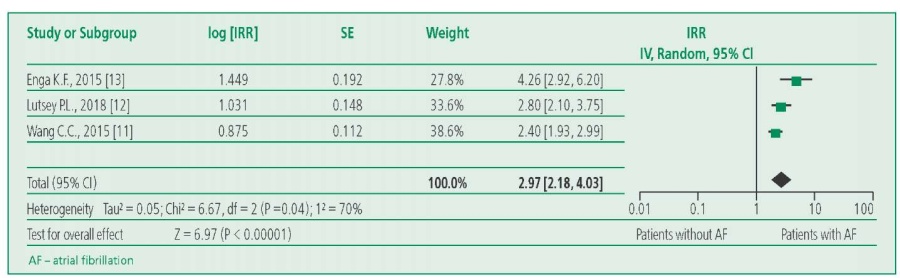
Figure 3. Forest plot of risk ratio (random effects model) results: deep vein thrombosis in patients with or without atrial fibrillation
Discussion
The major finding of our meta-analysis is that the risk of VTE is higher in patients with concomitant AF.
An important factor is the time of the onset of AF. P.L. Lutsey et al. have shown the increased risk of both DVT and PE in patients with AF during 6 months after diagnosis (hazard ratio [HR] 8.44; 95% CI 5.61-12.69) and (HR 4.50; 95% CI 2.61-7.77), respectively [12][13]. After 6 months the risk was no longer associated with DVT. It can be explained by such reasons as delay of anticoagulant treatment onset or rhythm and rate control strategy and concomitant hospitalization.
Moreover, P.L. Lutsey et al. [12] demonstrated that black patients exhibited a higher risk of VTE development within the first 6 months after the AF diagnosis (HR 2.49; 95% CI 1.55-3.74). But that may have been due to different (based on the race) access to medical care, likelihood of seeking treatment for minor illnesses, therapeutic intensity and anticoagulation control [17-19].
The population-based cohort study in Denmark has shown the similar results. In this study the 10-year cumulative risk of PE (1.30%, 95% CI 1.21-1.40) was higher than that of DVT (0.95%, 95% CI 0.87-1.04). The first days of onset AF played a crucial role. The aIRRs were 16.43 (95% CI 11.62-23.23) for PE and 8.20 (95% CI 5.42-12.42) for DVT during the first 30 days of follow-up. After this period of time the aIRR decreased markedly for both DVT and PE and remained close to unity after 1 year of follow-up. The aIRR remained increased in patients with provoked VTE and were only slightly lower for unprovoked ones [20].
Also, C.C. Wang et al. have shown that the risk of DVT was significantly higher in the AF group than in the non-AF group (2.98 vs 1.37 per 1000 person-years; adjusted HR 1.77; 95% CI 1.41-2.24). Also, the risk of PE was significantly higher in the AF group than in the non-AF group (1.55 and 0.46 per 1000 person-years; HR 2.68; 95% CI 1.97-3.64) [11].
Apparently, there are other risk factors and chronic diseases that can lead to an increased risk of VTE in patients with AF. K.F Enga et al. [13] differentiate VTE as provoked and unprovoked. The provoking factors were regarded as a recent surgery or trauma in the preceding 8 weeks, acute medical conditions (acute myocardial infarction, ischemic stroke, infectious disease), active cancer, immobilization (confinement to bed >3 days, wheelchair operating, long-distance trips >4 hours within 14 days before the event). The cases of unprovoked VTE were higher in the patients without AF (45%) than those with AF (31%). Active cancer and immobilization were the most frequent provoking factors in the patients without AF while acute medical conditions and immobilization were such factors for those with AF [13].
P. Noel et al. showed that such factors as elderly age, chronic cardiac failure and cardiomegaly in combination with AF may lead to DVT [14].
Prescription of oral anticoagulant therapy (vitamin K antagonists or novel oral anticoagulants) to the patients with AF can prevent stroke and systemic embolism (venous and arterial). According to some studies, the subsequent VTE risk was the lowest among the patients who were prescribed apixaban (HR 0.51, 95% CI 0.39-0.68) and dabigatran (HR 0.55, 95% CI 0.47-0.66) (especially during first 90 days of observation). At the same time, the risk was similar among those taking warfarin and rivaroxaban (HR 1.01, 95% CI 0.87-1.19) [21]. The decreasing of VTE risk can be an additional advantage of apixaban and dabigatran, besides a lower risk of bleeding observed in randomized clinical trials [22-25].
As opposite in a large multicenter study including 2,027 AF patients the ARAPACIS study only three DVT/PE event were registered during a median (IQR) follow-up time of 34.7 (22.0-36.0) months, resulting in a cumulative incidence of 0.65 per 1,000 person-years. Among patients included in the ARAPACIS study 47% aged 75 years and 55% were males. Hypertension was recorded in 82 % of patients, while diabetes and dyslipidaemia was recorded in 23% and 38% of cases, respectively. Cerebrovascular disease and heart failure affected 12% and 20% of cases. Globally, around 84% of patients were treated with an antithrombotic drug (oral anticoagulants, antiplatelets or both of them).
Study limitations. Lack of data on administering anticoagulants and platelet inhibitors, also high heterogeneity of the studies. Also, asymptomatic thromboembolic events might have come unnoticed and it was not always possible to determine the exact moment of AF onset. All these factors may affect the outcomes.
Conclusion
It can be concluded that the risk of VTE development might be increased for patients with concomitant AF and without AF in general population. It should be noted that other risk factors as well as chronic diseases in patients with AF are likely to increase the risk of VTE. It is obvious that this issue requires further research and other high-quality trials.
Relationships and Activities. None.
Funding: The study was performed with the support of the Sechenov University.
References
1. Benjamin EJ, Muntner P, Alonso A, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics 2019 update: a report from the American Heart Association. Circulation. 2019(10);139:e56e528. DOI:10.1161/CIR.0000000000000659.
2. Vadmann H, Nielsen PB, Hjortshøj SP, et al. Atrial flutter and thromboembolic risk: a systematic review. Heart. 2015;101(18):1446-55. DOI:10.1136/heartjnl-2015-307550.
3. Benjamin EJ, Blaha MJ, Chiuve SE, et al. American Heart Association Statistics C, Stroke Statistics S. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146-e603. DOI:10.1161/CIR.0000000000000485.
4. Rosamond WD, Folsom AR, Chambless LE, et al. Atherosclerosis Risk in Communities. Coronary heart disease trends in four United States communities. The Atherosclerosis Risk in Communities (ARIC) study 1987-1996. Int J Epidemiol. 2001;30(1):S17-22. DOI:10.1093/ije/30.suppl_1.s17.
5. Bikdeli B, Abou Ziki MD, Lip GYH. Pulmonary Embolism and Atrial Fibrillation: Two Sides of the Same Coin? A Systematic Review. Semin Thromb Hemost. 2017;43(8):849-63. DOI:10.1055/s-00361598005.
6. Kukla P, Dlugopolski R, Krupa E, et al. Electrocardiography and prognosis of patients with acute pulmonary embolism. Cardiol J. 2011;18(6):648-53. DOI: 10.5603/cj.2011.0028.
7. Barra SN, Paiva LV, Providencia R, et al. Atrial fibrillation in acute pulmonary embolism: prognostic considerations. Emerg Med J. 2013;31(4):308-12. DOI:10.1136/emermed-2012-202089.
8. Gustafsson C, Blombäck M, Britton M, et al. Coagulation factors and the increased risk of stroke in nonvalvular atrial fibrillation. Stroke. 1990;21(1):47-51. DOI:10.1161/01.str.21.1.47.
9. Kahn SR, Solymoss S, Flegel KM. Nonvalvular atrial fibrillation: evidence for a prothrombotic state. CMAJ. 1997;157(6):673-81.
10. Motoki H, Tomita T, Aizawa K, et al. Coagulation activity is increased in the left atria of patients with paroxysmal atrial fibrillation during the non-paroxysmal period: comparison with chronic atrial fibrillation. Circ J. 2009;73(8):1403-7. DOI:10.1253/circj.cj-09-0008.
11. Wang CC, Lin CL, Wang GJ, et al. Atrial fibrillation associated with increased risk of venous thromboembolism. A population-based cohort study. Thromb Haemost. 2015;113(1):185-92. DOI:10.1160/TH14-05-0405.
12. Lutsey PL, Norby FL, Alonso A, et al. Atrial fibrillation and venous thromboembolism: evidence of bidirectionality in the Atherosclerosis Risk in Communities Study. J Thromb Haemost. 2018;16(4):670679. DOI:10.1111/jth.13974.
13. Enga KF, Rye-Holmboe I, Hald EM, et al. Atrial fibrillation and future risk of venous thromboembolism: the Tromsø study. J Thromb Haemost. 2015;13(1):10-6. DOI:10.1111/jth.12762.
14. Noel P, Gregoire F, Capon A, et al. Atrial fibrillation as a risk factor for deep venous thrombosis and pulmonary emboli in stroke patients. Stroke. 1991;22(6):760-2. DOI:10.1161/01.str.22.6.760.
15. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3.0 [updated March 2022]. The Cochrane Collaboration, 2022 [cited 2021 Nov 10] Available from: https://training.cochrane.org/handbook/current.
16. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-5. DOI:10.1007/s10654010-9491-z.
17. Bhave PD, Lu X, Girotra S, et al. Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm. 2015;12(7):1406-12. DOI:10.1016/j.hrthm.2015.03.031.
18. Rao SR, Reisman JI, Kressin NR, et al. Explaining racial disparities in anticoagulation control: results from a study of patients at the Veterans Administration. Am J Med Qual. 2015;30(3):214-22. DOI:10.1177/1062860614526282.
19. Meschia JF, Merrill P, Soliman EZ, et al. Racial disparities in awareness and treatment of atrial fibrillation: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2010;41(4):581-7. DOI:10.1161/STROKEAHA.109.573907.
20. Sundbøll J, Hováth-Puhó E, Adelborg K, et al. Risk of arterial and venous thromboembolism in patients with atrial fibrillation or flutter: A nationwide population-based cohort study. Int J Cardiol. 2017;241:182-7. DOI:10.1016/j.ijcard.2017.04.081.
21. Lutsey PL, Norby FL, Zakai NA, et al. Oral anticoagulation therapy and subsequent risk of venous thromboembolism in atrial fibrillation patients. Curr Med Res Opin. 2019;35(5):837-45. DOI:10.1080/03007995.2018.1541445.
22. Connolly SJ, Ezekowitz MD, Yusuf S, et al. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139-51. DOI:10.1056/NEJMoa0905561.
23. Patel MR, Mahaffey KW, Garg J, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-91. DOI:10.1056/NEJMoa1009638.
24. Granger CB, Alexander JH, McMurray JJV, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-92. DOI: 10.1056/NEJMoa1107039.
25. Giugliano RP, Ruff CT, Braunwald E, et al. ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093-104. DOI:10.1056/NEJMoa1310907.
About the Authors
A. A. SokolovaRussian Federation
Anastasya A. Sokolova - eLibrary SPIN 2153-3542.
Moscow
A. A. Kudriavtseva
Russian Federation
Anna A. Kudriavtseva
Moscow
N. V. Kostokova
Russian Federation
Nina V. Kostokova
Moscow
M. P. Zaikina
Russian Federation
Margarita P. Zaikina
Moscow
Z. A. Gebekova
Russian Federation
Zarema A. Gebekova
Moscow
D. A. Napalkov
Russian Federation
Dmitry A. Napalkov - eLibrary SPIN 2894-5010.
Moscow
I. A. Zolotukhin
Russian Federation
Igor A. Zolotukhin - eLibrary SPIN 3426-2981
Moscow
Review
For citations:
Sokolova A.A., Kudriavtseva A.A., Kostokova N.V., Zaikina M.P., Gebekova Z.A., Napalkov D.A., Zolotukhin I.A. Risk of Venous Thromboembolic Complications in Patients with Atrial Fibrillation: a Systematic Review and Meta-analysis. Rational Pharmacotherapy in Cardiology. 2022;18(3):236-241. https://doi.org/10.20996/1819-6446-2022-06-02
















































