Scroll to:
Assessment of Drug Related Problems and Pharmacist Interventions in Inpatients with Cardiovascular Disease
https://doi.org/10.20996/1819-6446-2022-10-07
Abstract
Aim. To identify and evaluate the nature and incidence of drug-related problems (DRPs) and to manifest the role of a pharmacist in ensuring safe and efficient use of medications with cardiovascular disease patients by using PCNE Classification to assess and report drug-related problems.
Material and Methods. An Observational and Prospective study was conducted in a tertiary care hospital of medicine department of general and intensive/critical care units for a period of 6 months to identify and evaluate the nature and incidence of DRP’s and to manifest the role of a pharmacist in ensuring safe and efficient use of medications with cardiovascular disease patients by using PCNE Classification to assess and report drug-related problems.
Results. Of 94 Patient profiles were evaluated out of which 78 (82.9%) patient profiles were identified with 208 DRPs. Among 208, 140 (67.3%) drug interactions, 15 (7.2%) untreated indication, 12 (5.8%) adverse drug reactions, 10 (4.8%) drug use without indication, 8 (3.8%) drug underused, 8 (3.8%) duration of treatment too short, 5 (2.4%) dose unclear, 4 (1.9%) inappropriate drug form, 3 (1.4%) duration of treatment too long, 2 (1.0%) too many drugs prescribed for an indication, 1 (0.5%) drug overused. For 208 DRPs identified and provided with 74 interventions which includes 30 (41.6%) drug discontinuation, 24 (33.3%) addition of a new drug, 4 (5.55%) change of dosage form, and 14 (19.4%) decrease the dose.
Conclusion. The present study revealed that patients with cardiovascular diseases suffer from numerous DRPs that can be identified, resolved, or prevented to some extent by pharmacist intervention. Hence the study addresses the importance of clinical pharmacist in the management of DRPs among cardiovascular patients.
Keywords
For citations:
Biradar S.M., Kohima B., Nayak V., Nandikol S., Warad V., Byakod S.M., Hunasagi B.S., Awasthi S.R. Assessment of Drug Related Problems and Pharmacist Interventions in Inpatients with Cardiovascular Disease. Rational Pharmacotherapy in Cardiology. 2022;18(5):536-543. https://doi.org/10.20996/1819-6446-2022-10-07
Introduction
Drug-Related Problems (DRPs) are becoming predominant in cardiovascular disease patients with multiple medications in the current scenario. DRPs can be expressed as an event (or) circumstance involving the drug treatment, which interferes or potentially interferes with the patient in achieving an optimum outcome of medical care [1]. DRPs were categorized using PCNE classification (Pharmaceutical Care Network Europe Version 8.01) which is used globally to analyze the DRP’s and classify them under major categories as Adverse Reactions, Drug Choice Problem, Dosing Problem, Drug Use/Administration Problem, Drug Duration Problem, Inappropriate Drug Form, Interactions and Others [2]. DRPs may transpire at any stage of the medication process from prescription to follow-up of treatment. Most of the problems generally occur on administration, dispensing, and during the use of medication, but lack of proper follow-up and reassessment of medical treatment by a physician is also a major problem [1][3][4]. Drug-related problems are of major concern in health care because of increased cost, morbidity and mortality. DRPs is associated with prolonged length of hospitalization, increased economic burden, and an almost 2-fold increased risk of death [5][6]. An epidemiologic transition which is occurring in every part of the world, among all races, ethnic groups, and cultures has resulted in the global rise in cardiovascular disorders (CVD). Cardiovascular diseases are a group of disorders of the heart and blood vessels [7][8]. Cardiovascular disease is usually seen in middle-aged or elderly men and women. With the turn of the century, cardiovascular diseases (CVDs) have become the leading cause of mortality in India [9]. In comparison with the people of European ancestry, CVD affects Indians at least a decade earlier and in their most productive midlife years. For example, in Western populations only 23% of CVD deaths occur before the age of 70 years in India; this number is 52% [10]. According to the Global Burden of Disease study age-standardized estimates (2010), nearly quarters (24.8%) of all deaths in India are attributable to CVD. The most common incidence of cardiovascular diseases is Ischemic Heart Disease (IHD), Stroke, and Hypertensive Heart Disease whereas; atrial fibrillation incidence was less common in India when compared to western countries [11]. Even though pharmacotherapy in cardiovascular diseases can enhance well-being, its benefit can be compromised by drug-related problems (DRPs) [12][13]. The pharmacist is a substantial health care professional in the identification of a DRP, in the correct implementation of rational drug use principles by giving drug-related deliberate services and in the development and improvement of pharmaceutical care services by observing the patient during the treatment process [14]. Since early identification of the types and patterns of DRPs and the factors associated with them may enhance the prevention and management of DRPs. Categorizing and identifying drug-related problems will also enable the practitioner in collaboration with patient to construct a better care plan [7][9][15]. The goal of pharmaceutical care is to optimize drug therapy, achieve positive clinical outcomes within realistic economic expenditures, and improve patient's health-related quality of life [4][16]. The role of a pharmacist in Drug therapy Management (DTM) can prove to be the best to achieve therapeutic goals in patients and improves treatment outcomes by effective drug use and patient safety [17].
Material and Methods
An observational and Prospective study was conducted for six months in a tertiary care teaching hospital (1000 bed capacity), Vijayapura, on inpatients diagnosed with cardiovascular diseases who were admitted to the medicine department of general and intensive/critical care units (ICU/CCU). Being an observational study, the researchers individually and personally collected the data and studied in by the protocol, and made clinical pharmacist interventions wherever/whenever it was necessary. Study duration was divided into 3 stages as follows.
Stage 1: Review of literature and setting up of Protocol (Two months).
Stage 2: Data collection (Three months).
Stage 3: Result analysis and write-up (One Month).
Inclusion Criteria: Patients of both the gender above 18 years of age admitted to the hospital with cardiovascular diseases along with co-morbidities or without co-morbidities.
Exclusion Criteria: Discharges against medical advice, medico-legal cases, and patients who were not willing to participate in the study were excluded.
Source of data: Patient case files consist of demographic details, clinical characteristics, social history, Diagnosis, Drug dosages, duration of patient’s treatment, and Discharged drugs. Truven Micromedex online drug databases, PCNE classification, Standard Textbooks, Journals, Research articles and Newsletters.
Data collection and assessment: The data collected from case sheets were analyzed based on the process of classification, identification, and evaluation of DRP. We first categorized DRPs by using an established system developed by the Pharmaceutical Care Network Europe (PCNE) and possible interventions were done.
Statistical analysis: All the data were analyzed & presented by Percentages & Diagrams. Statistical analysis was done using Microsoft Excel and statistical software SPSS version 17 and P-value <0.05 was considered as statistically significant. Chi-square test was used to test for significant differences within the groups, which were categorized in the PCNE form such as the type, causes of the problem, intervention and outcome. Association be tween the number of drug prescribed, clinical/pharmacological risk factors and DRPs was found out by Pearson’s correlation coefficient.
Results
A total of 94 patients were followed out of which, 78 patients were intervened for having one or more drug related problems. Among 94 patients, the males were 54 (57.4%) predominance over females 40 (42.6%). Analysis of age-wise distribution showed that a maximum number of patients with DRP’s were among the age group between 51-65 years (40.4%) & minimum was >81years (6.3%) (Fig. 1). Risks factors influenced with DRPs like number of drugs, co-morbidities where as social history was not associated with the DRPs (Table 1, Fig. 2). Social history is a part of medical history addressing familial, occupational and recreational aspects; in this we included tobacco (gutka, chewable one), smoking (cigarettes) and alcohol.
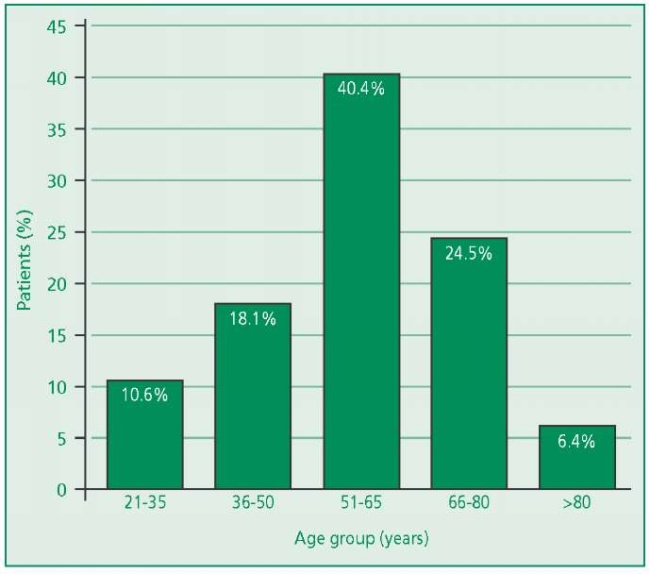
Figure 1. Distribution of patients according to age groups
Table 1. Risk factors significantly associated with drug-related problems
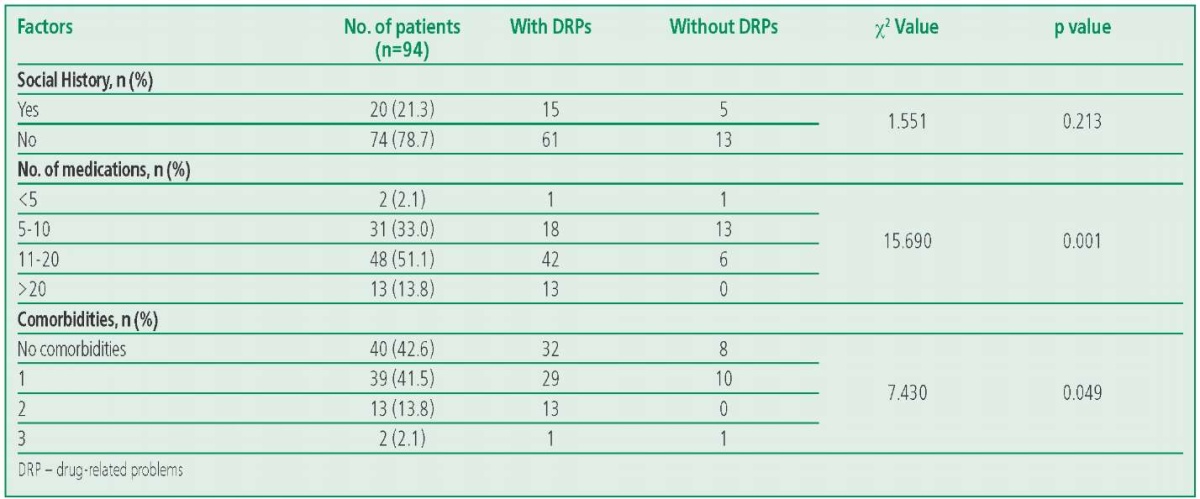
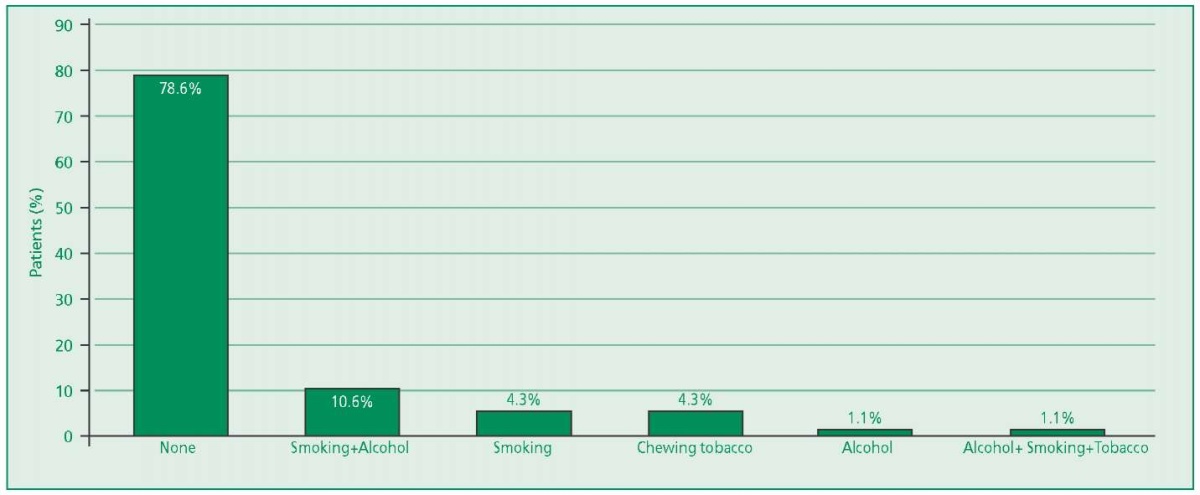
Figure 2. Distribution according to social habits
Distribution of subjects according to cardiovascular diseases
Out of 94 patients, frequently diagnosed diseases were Ischemic Heart Disease 48 (51.1%), followed by Hypertension 37 (39.4%), Myocardial Infraction 18 (19.1%), Ventricular Tachycardia/Failure 13(13.8%), Valvular Diseases 10 (10.6%), Acute Coronary Syndrome 8 (8.5%), Angina 7 (7.4%), Heart Failure 4 (4.3%), Atrial Fibrillation 3 (3.2%), and Dilated Cardiomyopathy 3 (3.2%) (Fig. 3).
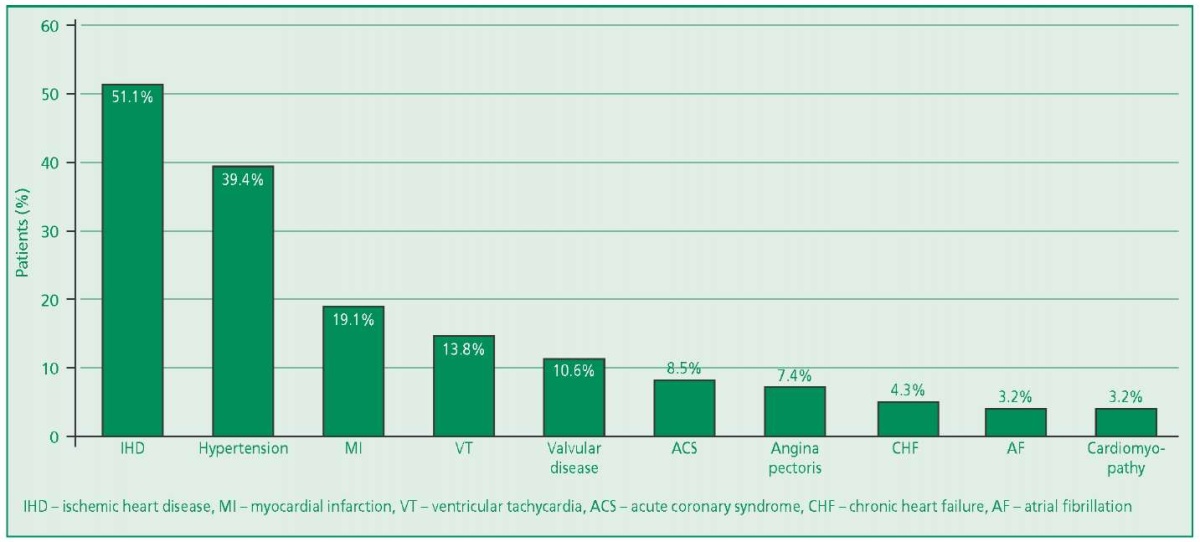
Figure 3. Distribution of cases according to cardiovascular diseases
Drug related problems evaluation
Evaluation of cases for DRPs
The results obtained at the end of the study were among 94 patients 78 (82.9%) patient profiles were identified with 208 DRPs. out of 208 DRPs, the most common were 140 (67.3%) Drug interactions, 15 (7.2%) Untreated indication, 12 (5.8%) Adverse drug reactions, 10 (4.8%) Drug use without indication, 8 (3.8%) Drug underused, 8 (3.8%) Duration of treatment too short, 5 (2.4%) Dose unclear, 4 (1.9%) Inappropriate drug form, 3 (1.4%) Duration of treatment too long, 2 (1.0%) Too many drugs prescribed for an indication, 1 (0.5%) Drug overused (Table 2).
Table 2. Types of drug related problems (n=208)

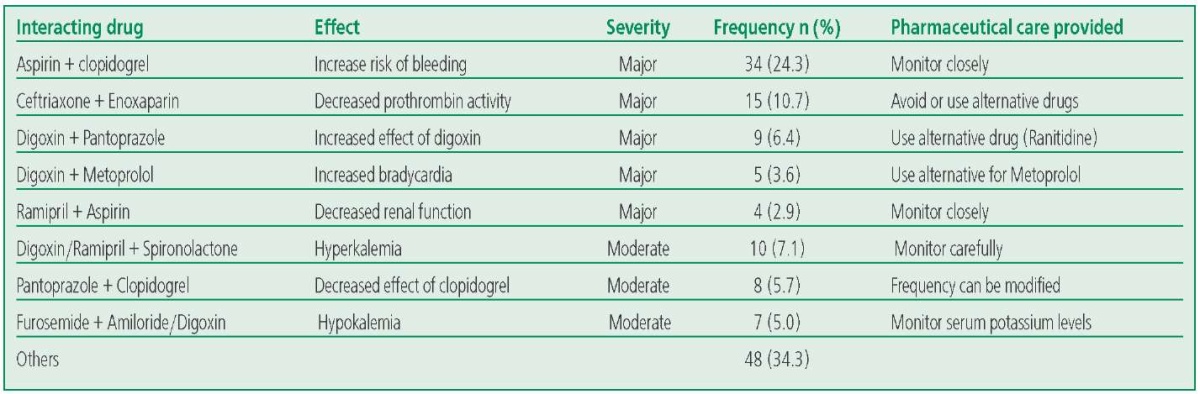
Drug Interactions
It was observed that 140 (67.3%) Drug interactions were more common among DRPs which accounts for 70 (50%) major drug interactions, 54 (38.5%) moderate drug interactions and 16 (11.4%) minor drug interactions (Table 3).
Table 3. Frequently occurring Drug Interactions
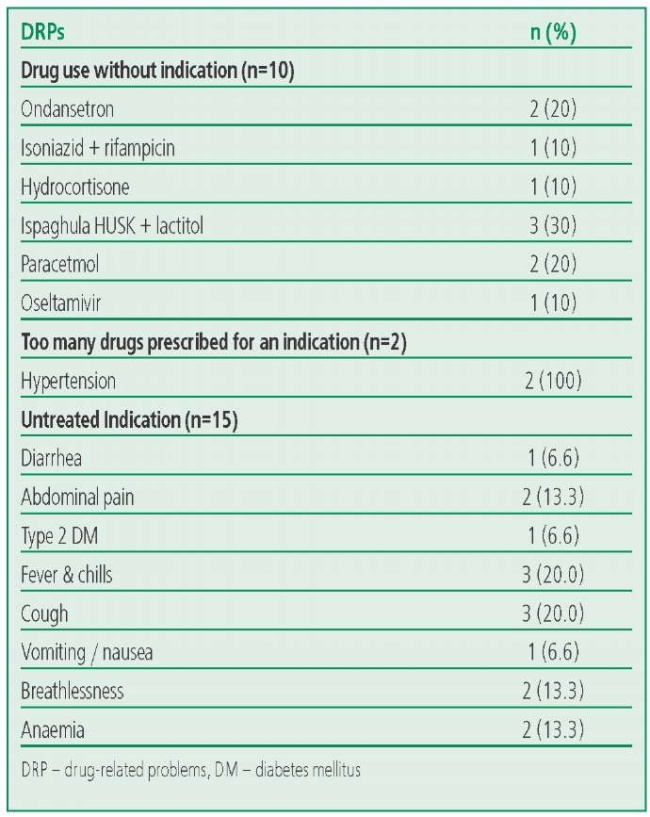
Drug Selection
The most common untreated indications were cough, fever & chills (20%), breathlessness, anemia, abdominal pain (13.3%) and diarrhea, vomiting/nausea (6.6%). Drug use without indication appeared to be 4.8% which adds chances of drug safety issues (Table 4).
Table 4. Drug selection
Adverse Drug Reactions
ADRs accounts for 5.8% of the total DRPs were observed. A combination of Digoxin & Spironolactone induces a ADR type of gynaecomasti (n=4), followed by Amlodepine induced Bilateral pitting edema (n=2), Clopidogrel induced Hematuria (n=5) and Alprazolam induced ADR of Slurred speech (n=1) (Table 5).
Table 5. Adverse drug reactions

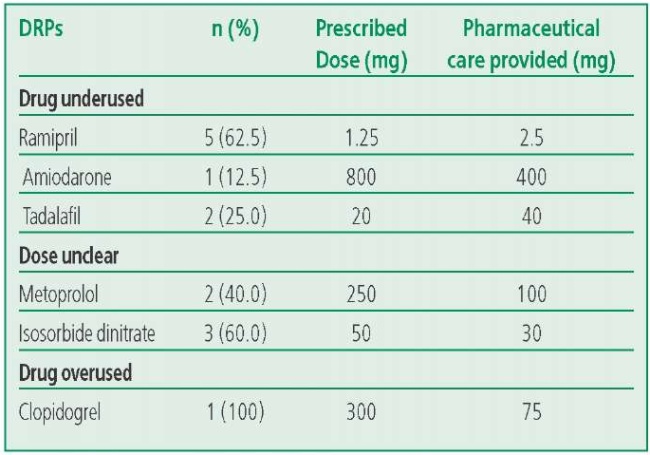
Dose selection
Drug underused accounts for 3.8% where the most common drug underused was Ramipril. Ramipril has prescribed 1.25 mg without diuretics where the standard prescribing dose must be 2.5mg when only Ramipril was administered. Dose unclear indicates 2.4% for the drugs Metoprolol & Isosorbide dinitrate where the prescribed dose was unclear with the standard doses. Drug overuse represents 0.5% In case of ACS, stroke, coronary artery disease; it was observed that clopidogrel was prescribed 150mg & 300 mg when it was used as monotherapy (Table 6).
Table 6. Dose selection
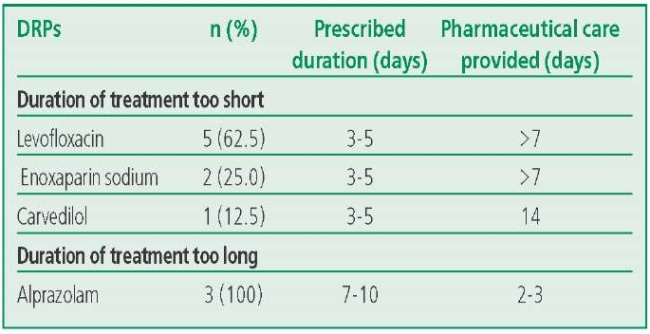
Treatment Duration
Duration of treatment too short represents 3.8%, Levofloxacin and Enoxaparin were prescribed only for 3-5 days whereas, Carvedilol was prescribed only for 3-5 days. Drug continuation was recommended in these cases. Duration of treatment too long accounts for 1.4% Alprazolam for anxiety associated depression, premenstrual syndrome, panic disorders, should be prescribed for 3-4 days but in the present study, it was administered for more than 7 days (Table 7).
Table 7. Treatment Duration
Pharmacist Interventions
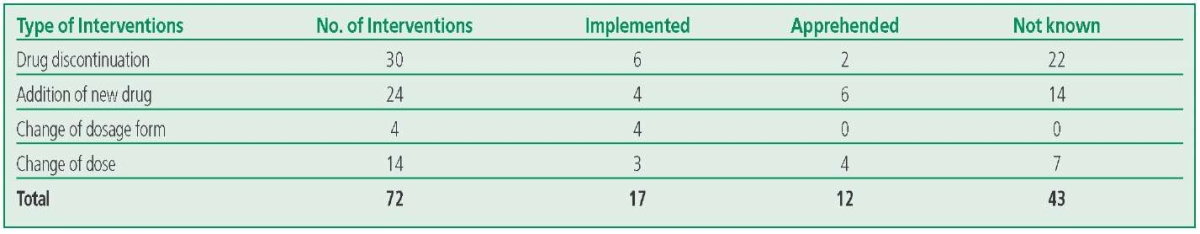
For 208 DRPs identified, we provided 74 interventions which includes 30 (41.6%) Drug discontinuation, 24 (33.3%) Addition of a new drug, 4 (5.55%) Change of dosage form and 14(19.4%) Decrease the dose. Out of 74 interventions proposed the acceptance of pharmacist’s interventions was found to be in 17 prescriptions. 12 recommendations were accepted but the therapy was not changed perhaps due to lack of proper information and in 43 cases the suggestions were neither suggested nor the drug therapy implemented (Table 8).
Table 8. Types of Pharmacist Interventions (n=72)
Discussion
In the present study male were predominant with CVDs compared to females, it may be due to as male are more prone to have CVDs (in Indian scenario). Advanced age and co morbid condition may contribute to the development of CVDs among the aged population. Risks factors influenced with DRPs like number of drugs, co-morbidities whereas; social history was not associated with the DRPs. A significant association between DRPs and without DRPs was done by chi-square test Which shows risk factors associated with drug therapy problems were due to usage of multiple medications and existing co morbid conditions. The incidences of DRPs were higher in males than females among the age groups 51-65 years. These results might be due to multiple drug regimens owing to their multiple co-morbidity and age related changes in pharmacokinetics and pharmacodynamics in elderly patients. Furthermore, majority of patients have one or more co-morbidities and also received more than 6 drugs during their admission thus increasing the likelihood of developing the drug related problems. Studies have shown that the number of drugs at admission and the number of clinical/pharmacological risk factors were both independent risk factors for the occurrence of DRPs [16][17].
Distribution of subjects according to cardiovascular diseases
The most often diagnosed CVDs were ischemic heart disease (including myocardial infarction) and hypertension followed by others. Factors might involved is Indian genetic trait, social habits and other risk factor ignorance.
Drug Interactions
The efficacy of the interaction increases when cardiovascular drugs like Clopidogrel are co-prescribed with proton pump inhibitors such as pantoprazole and Rabeprazole as both classes of drugs are metabolized by cytochrome P450 pathway [1][22]. Combination therapy is safe when indicated in a patient at high risk of GI bleeding, but they should also stop PPI therapy if it is not clinically indicated. The higher incidence of drug interactions in the study suggests that regular analysis of the patient case sheets including the drug therapy helps in identifying and preventing drug-related problems mainly the drug interactions [20][23]. Most of the drug interactions were due to anti- platelets, anti-coagulants, anti-hypertensive agents, GI drugs. The most commonly occurring drug interaction among the cardiovascular drugs includes aspirin, Clopidogrel, digoxin, atorvastatin, and anti-hypertensive agents such as amlodipine, furosemide, amiodarone, ramipril, spironolactone, metoprolol, and anticoagulants like warfarin, enoxaparin [1][12][16].
Drug Selection
These untreated indications were mostly due to their existing comorbid conditions like gastrointestinal diseases, respiratory diseases, bacterial or viral infections. Pharmacist interventions such as the addition of drugs like cough syrup (terbutaline, bromhexine, guaifenesin, menthol), paracetamol, probiotics, and ondansetron were recommended to such untreated indications. Few drugs were prescribed without indication such as ispaghula HUSK+lactitol, ondansetron, paracetamol, oseltamivir, hydrocortisone, rifampicin + isoniazid. There are no such existing conditions or symptoms to the patients where above-prescribed drugs are necessary. In such cases, drug withdrawal was recommended for possible circumstances.
Adverse Drug Reactions
Patients with hematuria should be closely monitored for the further occurrence of bleeding. Alprazolam-induced slurred speech was observed, dose depletion (0.25mg) was proposed. Gynecomastia was one of the ADRs which were occurred by digoxin and spironolactone. When both the drugs were administered together chances of gynecomastia were more predominant [21] [24]. Co-administration should be avoided in such cases & also de-challenging spironolactone and replaced by furosemide was recommended. Amlodipine induced pedal edema which was common in the elderly, dose reduction (2.5 mg) was recommended [11][12].
Dose selection
Drug underused accounts for 3.8% where the most common drug underused was Ramipril. In the case of Arterial Hypertension, Ramipril with diuretics dose should be 1.25 mg but in this study, Ramipril has prescribed 1.25 mg without diuretics where the standard prescribing dose must be 2.5 mg when only Ramipril was administered. Dose unclear indicates 2.4% for the drugs Metoprolol & Isosorbide dinitrate where the prescribed dose was unclear with the standard doses. Drug overuse represents 0.5% (See Table 6). In case of ACS, stroke, coronary artery disease; Clopidogrel must be prescribed 75 mg/day, when in combination with aspirin it can be 75-325 mg/day. In this study, it was observed that clopidogrel was prescribed 150 mg & 300 mg when it was used as monotherapy.
Treatment Duration
Duration of treatment too short represents3.8%. Levofloxacin for community-acquired pneumonia, COPD and skin infections whereas Enoxaparin in case of unstable angina, ACS &deep vein thrombosis should be administered for at least 7-10 days, where as in this study it was prescribed only for 3-4 days respectively. Carvedilol for congestive cardiac failure, MI, should be at least given for 2 weeks but the drug was prescribed only for 3-5 days. Drug continuation was recommended in these cases. Duration of treatment too long accounts for 1.4% (See Table 7). Alprazolam for anxiety associated depression, premenstrual syndrome, panic disorders, should be prescribed for 3-4 days but in the present study, it was administered for more than 7 days. Drug de-challenging was recommended as it may lead to side effects like drowsiness, tiredness, dizziness, and memory loss.
Pharmacist Interventions
This indicates that a clinical pharmacist can contribute to better patient care is involved in the health care team. The overall findings from the study were that pharmacists could identify some drug- related problems, prompt and proper intervention will help in achieving better patient care that can lead to improving the quality of care and drug therapy.
Conclusion
The present study showed that patients with cardiovascular diseases suffer from a numerous DRPs that can be identified, resolved, or prevented to an extent by clinical pharmacist intervention. The therapeutic outcome of the patient can be improved by early detection and documentation of DRPs.
Following the ESC guidelines for the prescription and treatment would help to minimize/reduce the DRPs. Routine medication review, patient adherence to the therapy and reactive pharmacist intervention are strongly recommended to improve the treatment outcome of patients with cardiovascular diseases. Hence the current study clearly showed that pharmaceutical care and clinical pharmacist services have tremendous scope to improve the patients' quality of life in cardiovascular diseases.
Relationships and Activities. None.
Funding: The study was performed with the support of the SSM College of Pharmacy and Research Centre and Shri B.M. Patil Medical College Hospital and Research Centre.
References
1. Javedh S, Sandeep B, Shastry CS. Assessment of Drug Related Problems in Patients with Cardiovascular Diseases in a Tertiary Care Teaching Hospital. J Pharm Care. 2014;2(2):70-6.
2. PCNE Classification V8.01,2017-6-15 [cited 2021 Jan 10]. Available from: https://www.pcne.org/upload/files/215_PCNE_classification_V8-01.pdf.
3. Wincent MM, Potrilingam D, Anagha V. Assessment of Drug Related Problems in patients with Chronic diseases in the general medicine units of a tertiary care hospital. Int J Pharm Pharm Sci. 2017;9(12):194-200. DOI:10.22159/ijpps.2017v9i12.21660.
4. Sharma A, Baldi A, Sharma D. Assessment of drug related problems among Diabetes and Cardiovascular disease patients in a tertiary care teaching hospital. Pharm Aspire. 2018;10(1):7-12. DOI:10.4314/tjpr.v15i10.29.
5. Gashaw B, Mequanent K, Masho T. Assessment of Drug Related Problems and its Associated Factors among Medical Ward Patients in University of Gondar Teaching Hospital, Northwest Ethiopia: A Prospective Cross-Sectional Study. J Basic Clin Pharma. 2017;8(S1):S16-S21.
6. Gobezie T, Belay Y, Elias Ali Y, et al. Drug Therapy Problems among patients with Cardiovascular Diseases in Felege Hiwot Referral Hospital North East Ethiopia. International Journal of Pharmacy Teaching and Practices. 2014;5(5):989-96. DOI:10.22270/jddt.v9i2-s.2439.
7. Tegegne G, Yimam B, Yesuf E. Drug Therapy Problem among patients with Cardiovascular Disease in Felege Hiwot Referral Hospital. Int J Pharm Teach Pract. 2014;5(3):989-96.
8. Gizaw K, Dubale M. Drug Related Problems and Contributing Factors among Adult Ambulatory Patients with Cardiovascular Disease at Gebretsadik Shawogeneral hospital. Journal of Natural Sciences Research. 2017;7(1):2224-3186.
9. Chauhan S, Aeri B. Prevalence of Cardiovascular disease in India and its economic impact. Int J Sci Res Publ. 2013;3(10):2250-3153.
10. Dorairaj P, Panniyammakal J, Ambuj R. Cardiovascular disease in India Current epidemiology and future directions. Circulation. 2016;1(1):1605-20. DOI:10.1161/CIRCULATIONAHA.114.008729.
11. Soumya S, Ramakrishna P, Vidya S, et al. Pattern of pharmacotherapy and assessment of drug related problems in Ischemic Heart Disease patients. Int Res J Pharma. 2019;10(3):136-43. DOI:10.7897/2230-8407.100392.
12. Rani RA. Drug Related Problems And Reactive Pharmacist Interventions for Inpatients Receiving Cardiovascular Drugs. IJBMSP. 2013;3(2):42-8.
13. Olatz U, Olivia F, Sonia L, et al. Patient risk factors for developing a drug related problem in a cardiology ward. Ther Clin Risk Manag. 2015;11:9-15. DOI:10.2147/TCRM.S71749.
14. Laika G, Arijana M, Bilgen B. Pharmacist intervention in drug related problems for patients with cardiovascular disease in selected community pharmacies in Northern Cyprus. Trop J Pharm Res. 2016;15(10):2275-81. DOI:10.4314/tjpr.v15i10.29.
15. Murray M, Ritchey M, Wu J, et al. Effect of a pharmacist on Adverse Drug Events and Medication Errors in Outpatients with Cardiovascular Disease. Arch Intern Med. 2009;169(8):757-63. DOI:10.1001/archinternmed.2009.59.
16. Sai Hamsini L, Priyanka G, Chandralekha D, et al. A study to assess drug related problems in patients with Cardiovascular Diseases in a tertiary care teaching hospital. J Drug Del Ther. 2019;9(2):20-7. DOI:10.22270/jddt.v9i2-s.2439.
17. Prajapati A, Shrikalp D. Drug Therapy Management of Cardiovascular Disease patients admitted to Intensive Care Units of Tertiary Care Hospitals. Indian J Pharm Prac. 2015;8(1):13-8. DOI:10.5530/ijopp.8.1.4.
18. Sushil G, Ramesh G, Kumar G, et al. Emerging risk factors for disease: Indian context. Indian J Endocrinol Metab. 2013;17(5):806-14. DOI:10.4103/2230-8210.117212.
19. Bela S, Prashant M. Surveillance of Cardiovascular disease risk factors in India: The need and scope. Indian J Med Res. 2013;132(5):634-42. DOI:10.4103/0971-5916.73420.
20. Devarashetty V, Praveen A, Manjunath R. Potential Drug-Drug interaction among Ischemic Heart Disease patients at a tertiary care hospital. Natl J Physiol Pharm Pharmacol. 2020;10(7):557-62. DOI:10.5455/njppp.2020.10.12389201926042020.
21. Yaschilal M, Belanyeh G, Amberbir A. A prospective observational study of drug therapy problems in medical ward of a referral hospital in northeast Ethiopia. BMC Heath Services Research. 2018;18(1):808. DOI:10.1186/s12913-018-3612-x.
22. Punniyakotti S, Nimisha. A retrospective observational study on Drug Related Problems in patients with Rheumatic Heart Disease. Int J Res Pharma Sci. 2018;10(1):135-9. DOI:10.26452/ijrps.v10i1.1789.
23. Yirga L, Kabaye K, Tesfaye D. Drug Therapy Problems and contributing factors in the management of Heart Failure patients in Jimma University specialised hospital Southwest Ethiopia. PLoS One. 2018;13(10):e0206120. DOI:10.1371/journal.pone.0206120.
24. Omboni S, Caserini M. Effectiveness of Pharmacist’s intervention in the management of cardiovascular disease. Open Heart. 2018;5(1):e000687. DOI:10.1136/openhrt-2017-000687.
About the Authors
S. M. BiradarIndia
Siddaruda M. Biradar
Vijayapur
B. Kohima
India
Kohima Bonthu
Vijayapur
V. Nayak
India
Vishwanath Nayak
Vijayapur
S. Nandikol
India
Sunanda Nandikol
Vijayapur
V. Warad
India
Vijaykumar Warad
Vijayapur
S. M. Byakod
India
Sharanabasappa M. Byakod
Vijayapur
B. S. Hunasagi
India
Basavaraj S. Hunasagi
Vijayapur
S. R. Awasthi
India
Santhosh R. Awasthi
Vijayapur
Review
For citations:
Biradar S.M., Kohima B., Nayak V., Nandikol S., Warad V., Byakod S.M., Hunasagi B.S., Awasthi S.R. Assessment of Drug Related Problems and Pharmacist Interventions in Inpatients with Cardiovascular Disease. Rational Pharmacotherapy in Cardiology. 2022;18(5):536-543. https://doi.org/10.20996/1819-6446-2022-10-07
















































