ORIGINAL STUDIES
Aim. To determine clinical, laboratory, and instrumental factors associated with no-reflow phenomenon in patients with myocardial infarction in the work of cardiology service of the emergency hospital.
Material and methods. A database of 2090 patients diagnosed with acute coronary syndrome and consecutively admitted to a regional vascular center was established for the study. Following percutaneous coronary intervention and assessment of coronary blood flow using the TIMI scale, 59 patients had the no-reflow phenomenon; these patients formed Group 1. Group 2 (n=149) was formed randomly from the remaining 2031 patients with final coronary blood flow TIMI 3. A comparative analysis of clinical, demographic, laboratory, and instrumental data between the two groups was performed, along with an assessment of factors influencing the development of the no-/slow-reflow phenomenon. Statistical analysis was performed using STATISTICA software (data analysis software system), version 10, StatSoft, Inc., using both parametric and non-parametric analysis methods.
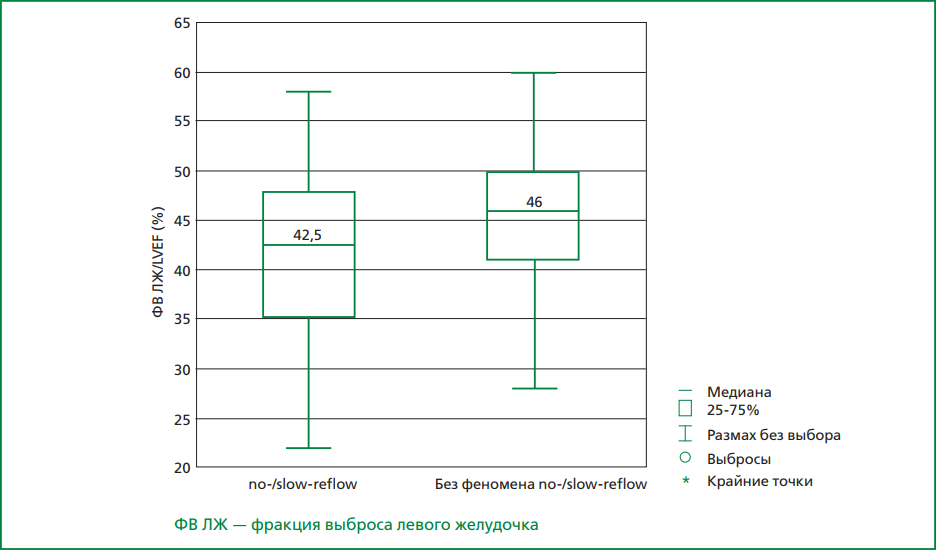
Results. In Group 1 diabetes mellitus was observed in 42.4% of patients compared to 22.8% in Group 2, p=0.003. Laboratory tests showed that the mean blood leukocyte count was 10.9×109/L in Group 1 and 9.5×109/L in Group 2, p=0.0015; absolute neutrophil count was 8.4×109/L and 6.6×109/L, respectively, p=0.0003. The mean left ventricular ejection fraction was 42% in Group 1 and 45% in Group 2, p=0.0015. Electrocardiographic changes in the anterior wall of the left ventricle were detected in 59% of Group 1 patients and 50% of Group 2 patients, p=0.018. Proximal lesions of the infarct-related artery were identified in 88% of Group 1 patients and 40% of Group 2 patients, p<0.0001.Binary logistic regression analysis revealed independent risk factors for the development of the no-/slowreflow phenomenon: level of infarct-related artery lesion [OR=3.33; 95% CI: 1.67-6.57; p<0.001], left ventricular ejection fraction [OR=1.1; 95% CI: 1.04-1.17; p<0.001], and time from pain onset to revascularization [OR=1.03; 95% CI: 0.95-0.996; p=0.02].
Conclusion. Prolonged total myocardial ischemia time, the presence of diabetes mellitus, lower left ventricular ejection fraction, elevated blood leukocyte and neutrophil counts, anterior localization of myocardial infarction, and more proximal occlusion of the coronary artery are associated with the development of the no-/slow-reflow phenomenon in patients with myocardial infarction in real clinical practice.
Aim. To study new possibilities of the potential of speckle tracking echocardiography for detecting early subclinical cardiotoxicity of chemo- and targeted therapy.
Material and methods. 150 patients with a verified oncological diagnosis, with a very high or high risk of cardiotoxicity, determined by the Mayo Clinic scale, were included in the prospective observational study at the Department of Hospital Therapy No. 1 of the Russian Medical University of the Ministry of Health of Russia in 2021-2023. All enrolled patients were recommended to take a fixed combination of the ACE inhibitor perindopril and the beta-blocker bisoprolol (5+5 mg) 5-7 days before the start of chemo-targeted therapy. Patients with a very high risk of cardiotoxicity who were diagnosed with ischemic chronic heart failure or stable coronary artery disease, or post-myocardial infarction, were additionally recommended to take long-acting trimetazidine OD at a dose of 80 mg once daily. At the second visit, the main group (n=84, receiving cardioprotective drugs) and the comparison group (n=66, not receiving cardioprotective drugs) were formed. All patients at the time of inclusion in the study, as well as 1, 3, 6, 9 and 12 months after the start of antitumor therapy, underwent the following assessment: collecting complaints, anamnesis data, physical examination, ECG registration in 12 standard leads, and a two-dimensional echocardiogram with the measurement of left ventricular (LV) global longitudinal strain (GLS).
Results. Primary drug prophylaxis in cancer patients with high and very high risk of cardiotoxicity was associated with a 2.7-fold decrease in significant cardiovascular complications. The development of chronic heart failure in the main group was noted 7 times less frequently than in the comparison group (n=1 (1.2%) vs n=7 (10.6%), p<0.05), a decrease in GLS LV 2.6 times (n=5 (5.9%) vs n=13 (19.7%), p<0.05). During the observation of oncological patients receiving chemo- and targeted therapy, it was found that a specific pattern, previously not described, was revealed in patients with developed systolic dysfunction upon visual assessment of the longitudinal strain of the LV. A decrease in contractility was noted in all LV basal segments, visually displayed by a pale or even blue color along the circumference of the diagram, with the presence of compensatory hyperkinesia of LV apical segments. LV strain reduction in the basal segments along the circumference of the outer part of the polar diagram >-18%, compensatory hyperkinesia of LV apical segments contractility <-18% in the inner part of the diagram compared to the initially determined values of the LV longitudinal strain before the start of antitumor therapy is an early, preclinical sign of cardiotoxicity.
Conclusion. The detection of typical changes in local longitudinal strain should be considered as an early sign of cardiotoxicity with a subsequent change in treatment tactics: temporary or permanent withdrawal of the drugs that caused cardiovascular complications, the appointment of cardioprotective therapy with ACE inhibitors, beta-adrenergic blockers and myocardial cytoprotectors.
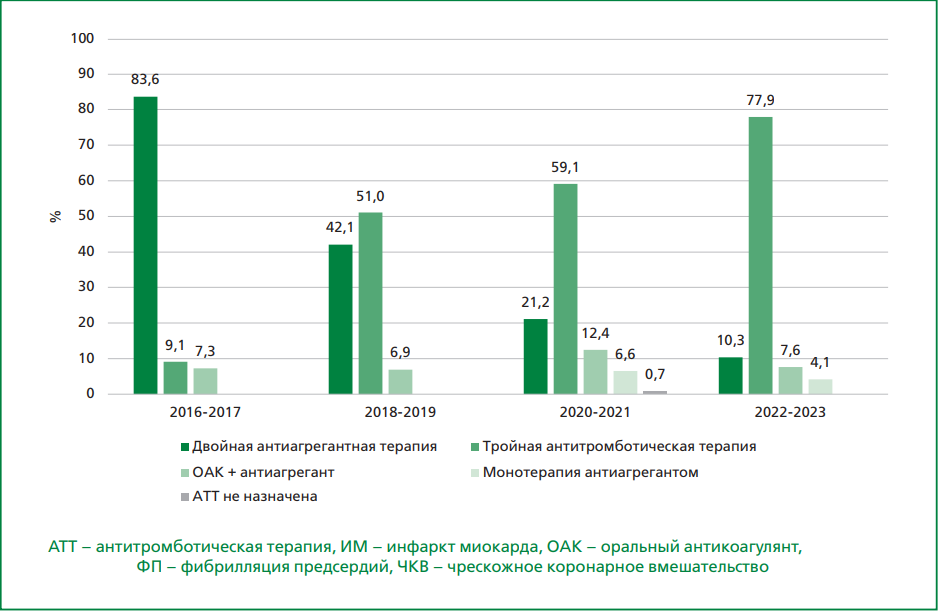
Aim. To analyse the dynamics of prescribing triple antithrombotic therapy (TATT) at discharge (TATT: oral anticoagulant (OAC) + two antiplatelet agents) in patients with atrial fibrillation (AF) and acute myocardial infarction (MI) between 2016-2023, as well as the alignment of clinical practice with the clinical guidelines of the European Society of Cardiology (ESC) and the Russian Society of Cardiology (RSC).
Material and methods. A retrospective analysis was conducted on 813 patients with AF and acute MI, divided into four groups based on hospitalisation period: 2016-2017 (n=104), 2018-2019 (n=256), 2020-2021 (n=239), 2022-2023 (n=214). The frequency and composition of ATT prescriptions were assessed, along with their compliance with current guidelines. Due to the absence of RSC guidelines before 2020, ATT compliance was assessed against the 2015 ESC guidelines for non-ST-segment elevation acute coronary syndrome (NSTE-ACS), the 2017 ESC guidelines for ST-segment elevation myocardial infarction (STEMI), and the 2016 ESC guidelines for AF. After 2020, compliance was evaluated against the 2020 RSC guidelines for the same conditions.
Results. Among patients not undergoing percutaneous coronary intervention (PCI), OAC + antiplatelet therapy was prescribed to 10.2% in 2016-2017 and 13.5% in 2018–2019, aligning with the 2016 ESC guidelines for AF. Among PCI-treated patients, TATT was prescribed in 9.1% of cases in 2016-2017 and 51.0% in 2018-2019, consistent with ESC guidelines. In non-PCI patients, the correct OAC + antiplatelet combination was prescribed to 17.2% in 2020-2021 and 27.5% in 2022-2023. TATT at discharge was prescribed to 48.7% of PCI-treated NSTE-ACS patients in 2020-2021 and 72.5% in 2022-2023, aligning with the 2020 RSC guidelines for NSTE-ACS. The combination of OAC + antiplatelet therapy for PCI-treated STEMI patients was prescribed in 13.3% of cases in 2020-2021 and 8.6% in 2022-2023, consistent with the 2020 RSC guidelines for STEMI. Overall, OAC use increased from 16.3% in 2016-2017 to 87.9% in 2022-2023.
Conclusion. The study demonstrates significant progress in OAC and TATT prescription. However, a gap remains between clinical practice and guidelines, particularly in the composition of combination therapy at discharge.
PAGES OF RUSSIAN NATIONAL SOCIETY OF EVIDENCE-BASED PHARMACOTHERAPY
Aim. To assess real-world practice in the use of invasive diagnostic and treatment methods in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS) within the registry of the regional vascular centre.
Material and methods. The study included 136 patients consecutively admitted on an emergency basis to the vascular center in Sergiyev Posad between October 2018 and March 2019 with a diagnosis of NSTE-ACS. The mean age was 63±11 years, and 61% were male.
Results. All patients underwent coronary angiography (CAG) as soon as possible after hospital admission (less than 2 hours). None of the patients had absolute contraindications for percutaneous coronary intervention (PCI). All 136 patients were divided into 3 groups based on the chosen invasive treatment strategy: patients who did not undergo PCI at the inpatient stage of treatment and with long-term follow-up — 69 people (50.7%; group 1); patients who underwent PCI during the current hospitalisation — 50 people (36.8%; group 2); patients who underwent delayed PCI after the current hospitalisation — 17 people (12.5%; group 3). The decision to perform PCI was not influenced by the disease patterns or the GRACE risk score. The results of the CAG showed that patients in group 3 had three-vessel coronary artery disease significantly more often than in groups 1 and 2 (59% vs 22% and 34%, p=0.001). Regression analysis showed that the detection of damage to only one coronary artery significantly increased the likelihood of PCI. This probability progressively decreased as the extent of CAD increased.
Conclusion. In the regional vascular centre, in-hospital PCI was performed in only 36% of patients diagnosed with NSTE-ACS. When deciding on PCI, physicians were primarily guided not by the degree of risk of cardiovascular complications, as required by clinical guidelines, but rather by the technical feasibility and safety of the procedure.
CURRENT QUESTIONS OF CLINICAL PHARMACOLOGY
The article discusses the results of randomized controlled trials and some observational studies that define the current understanding of the role of rivaroxaban in the prevention of cardioembolic complications in patients with atrial fibrillation (AF). According to the results of the randomized controlled trial ROCKET AF, in patients with non-valvular AF, rivaroxaban is at least as effective as warfarin. At the same time, while the rates of major and clinically significant non-major bleeding were comparable, fatal bleeding and bleeding in critical organs (including intracranial bleeding) were less frequent in the rivaroxaban group, whereas clinically relevant gastrointestinal bleeding occurred more often. Overall, the rate of major gastrointestinal bleeding increased by 10 cases per 1,000 treated patients per year in the rivaroxaban group, and its occurrence did not lead to the need for large-volume blood transfusions or an increased risk of death. Similar clinical effects can be expected in various patient categories, including those with impaired kidney function (down to a creatinine clearance of 15 mL/min) and elderly patients. According to accumulated evidence, rivaroxaban reduces the risk of coronary thrombosis after coronary stenting and should be combined with one antiplatelet agent (mainly clopidogrel) in this case. According to the results of the X-VERT study, rivaroxaban appears to be an effective and safe alternative to vitamin K antagonists during cardioversion and may allow for rapid cardioversion in hemodynamically stable patients with paroxysmal non-valvular AF. Due to the lack of an available laboratory monitoring method and significant variations in drug concentration in the blood among those receiving rivaroxaban, studies on bioequivalence with determination of anti-Xa activity in the blood are particularly important for its generics. Data on the similar composition of tablets, comparable dissolution kinetics and bioequivalence are available, in particular, from the Russian generic rivaroxaban Zinacoren.
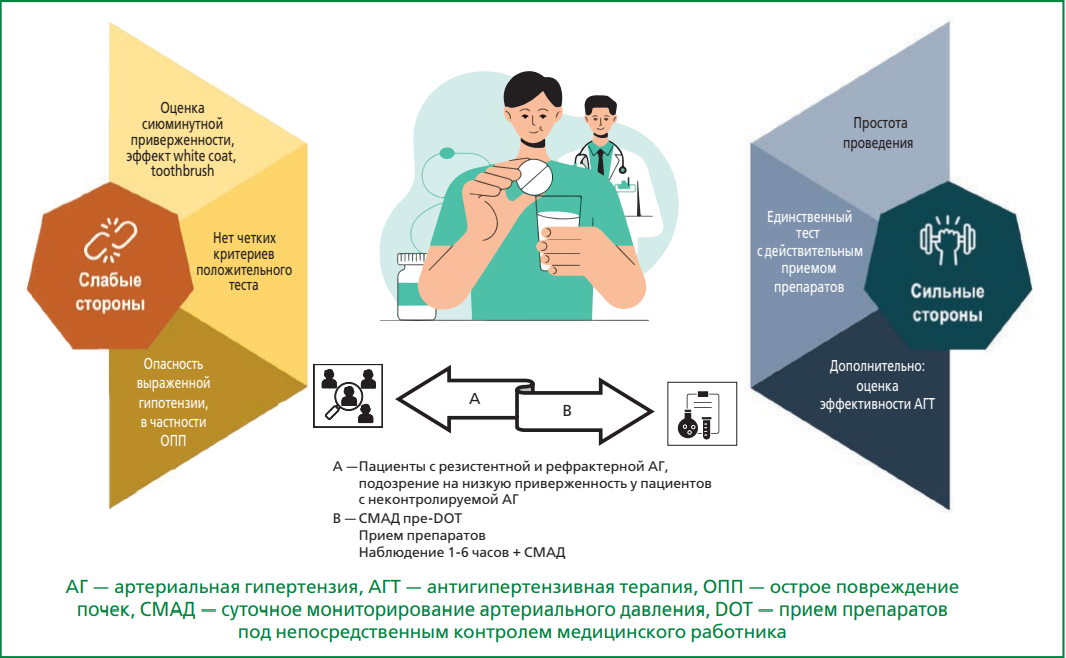
Low adherence to therapy is one of the main causes of pseudo-resistant arterial hypertension (AH), associated with an increased risk of cardiovascular complications and higher direct and indirect medical costs. Adherence assessment is a crucial step in the management of patients with uncontrolled AH, particularly when therapeutic resistance is suspected. There is no "gold standard" for assessing therapy adherence. Therefore, beyond indirect methods (though simple, they are relatively unreliable), direct approaches are increasingly being utilized. These include witnessed medication intake by medical personnel — conducted alongside repeated ambulatory blood pressure monitoring using portable devices or repeated measurements by a specialist — and therapeutic drug monitoring of medications or their metabolites in biological fluids using ultra-high-performance liquid chromatography-tandem mass spectrometry. This narrative review summarizes key findings from studies on the application of these methods, outlines their respective advantages and limitations, and provides practical recommendations for their integration into everyday clinical practice. Early and simultaneous implementation of these strategies can help avoid unnecessary complex and costly diagnostic procedures in some cases and allows for more accurate identification of truly resistant AH – a patient group of scientific and clinical relevance. The use of these approaches improves the cost-effectiveness of treatment, helps uncover non-medical barriers to adherence, and strengthens the physician–patient relationship.
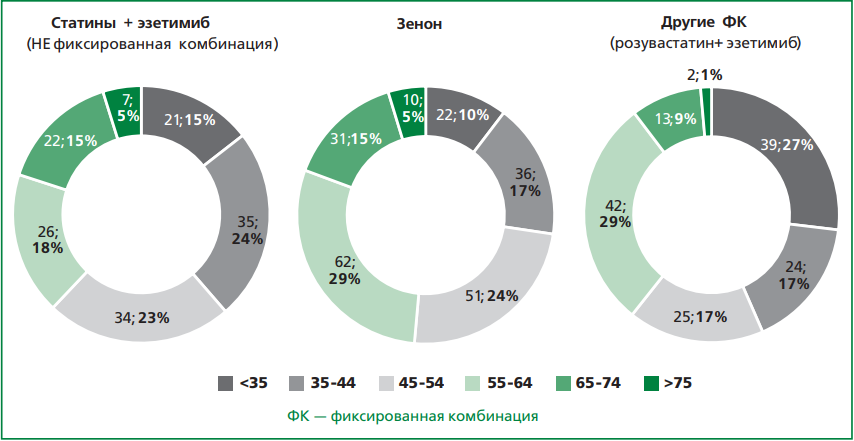
Aim. To study the adequacy and effectiveness of lipid-lowering therapy (LLT) prescribed to patients with heterozygous familial hypercholesterolemia (HeFH), including fixed-dose combinations (FDC) of rosuvastatin with ezetimibe, as well as the frequency of achieving target low-density lipoprotein cholesterol (LDL-C) levels.
Material and methods. The clinical and demographic data of 3151 patients with HeFH at high or very high cardiovascular risk from the RENAISSANCE registry were retrospectively analysed. Among the 1612 individuals receiving LLT, 477 patients were treated with a combination of rosuvastatin at various doses and ezetimibe 10 mg daily, either as a free combination or as a FDC.
Results. The median age of the patients was 46.0 [32.0; 57.0] years. The median LDL-C level was 6.4 [5.3; 7.8] mmol/L. Although LLT was recommended to all participants, approximately half (49%, n=1539) were not receiving treatment. Among the 1612 patients on LLT, 44% (n=703) received statin monotherapy, and 43% (n=697) were treated with a combination of statins and ezetimibe. Of the 477 patients taking rosuvastatin with ezetimibe, the majority were active adults of working age (35-64 years): 335 (80%) vs 86 (20%), p <0.05. Most patients preferred taking rosuvastatin with ezetimibe in the FDC: 357 (74.8%) vs 120 (25.2%), p <0.05. Among those on FDC, a significantly higher proportion used Zenon® compared to other FDCs: 44.4% (n=212) vs 30.4% (n=145), p <0.05. A significant reduction in LDL-C was observed compared to baseline: 61% in the free combination group and 65% in the FDC group, including a 67% reduction in the Zenon® subgroup (p <0.001). The rate of achieving LDL-C targets among high/very high cardiovascular risk patients was lower in the free combination group compared to the FDC group, with the highest rates observed among Zenon® users: 5.8% (n=7), 17.9% (n=26), and 21.7% (n=46), respectively (p <0.01).
Conclusion. Among patients with НeFH, the use of a FDC of rosuvastatin and ezetimibe is associated with higher treatment adherence and a greater likelihood of achieving target LDL-С levels.
ASSOCIATED PROBLEMS OF CARDIOLOGY
Aim. To study heart rate variability (HRV) parameters in patients with systemic sclerosis (SSc) and their relationship with disease characteristics and therapy.
Material and methods. A study included 48 SSc patients and 43 healthy individuals. HRV was assessed using electrocardiography (ECG) data recorded at rest during quiet breathing (a 5-minute ECG fragment) and ambulatory 24-hour ECG monitoring.
Results. According to 5-minute ECG recordings, in patients with SSc, an increase in heart rate (p=0.023) and changes in HRV frequency parameters were detected compared with the control group: a decrease in HFlog and HFn.u. (p=0.046 and p=0.027, respectively), an increase in LF (p=0.018) and the ratio LF/HF (p=0.016). According to ambulatory ECG monitoring data, patients with SSc have increased heart rate, decreased SDNNidx and pNN50 during the entire recording period and during the daytime, and a statistically significant decrease in most HRV parameters (meanNN, SDNN, SDNNidx, rMSSD and pNN50) at night. According to 5-minute ECG recordings, a relationship was found between heart rate (meanRR and meanHR) and the duration of Raynaud's syndrome (R=0.31, p=0.034; R=-0.30, p=0.043). In the presence of a history of heart damage in patients with SSc, according to ambulatory monitoring data, lower SDNNidxall, SDNNidxday, SDNNidxnight, pNN50night were noted, according to 5-minute ECG recordings — lower values of total power, LFmc2, LFlog, SD2. In the presence of lung damage, there is a higher heart rate according to meanRR, meanHR and meanNNday (according to 5-minute and ambulatory ECG recordings). Correlation between C-reactive protein (CRP) level of and SD2/SD1 were revealed according to 5-minute ECG recordings (R=-0.419, p=0.015), DFAα1 (R=-0.419, p=0.015). Patients with SSc taking calcium channel blockers (CCB) had higher values of HRV time parameters according to ambulatory ECG monitoring (p<0.05).
Conclusion. SSc patients exhibited reduced frequency-domain, time-domain, and nonlinear HRV parameters in both short-term and 24-hour ECG recordings. A potentially unfavorable relationship was identified between nonlinear HRV parameters and C-reactive protein (CRP) levels, as well as correlations of heart rate (HR) with Raynaud’s syndrome duration, and HRV with lung and heart involvement. CCB therapy was associated with improved circadian rhythm of HRV.
CLINICAL CASE
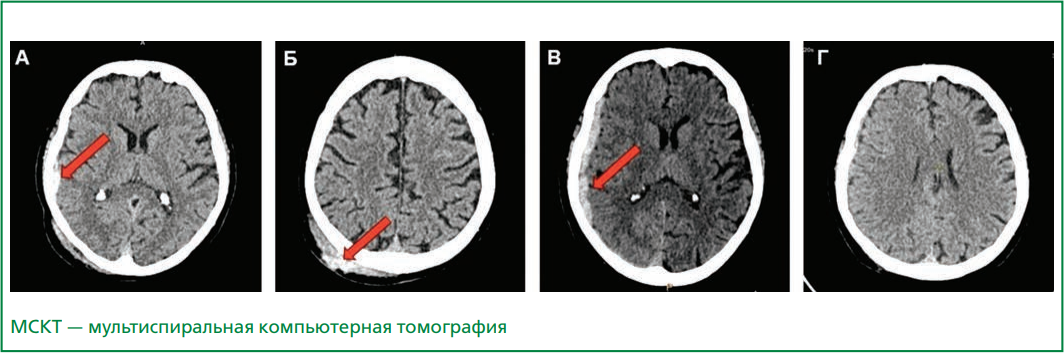
Aim. To evaluate the safety and efficacy of the non-immunogenic staphylokinase in a patient with a massive high-risk pulmonary embolism (PE) with subdural hematoma.
Material and methods. Non-immunogenic staphylokinase (Fortelyzin®, LLC “SuperGene”, Russia) is an original thrombolytic drug with high fibrin selectivity and minimal risk of bleeding. A clinical case of the non-immunogenic staphylokinase usage at a dose of 15 mg as a single bolus in an elderly patient with massive high-risk PE with subdural hematoma is presented.
Results. Thrombolytic therapy with the non-immunogenic staphylokinase was performed in an 85-years old female with very high mortality risk PE (PESI class V) associated with acute subdural lamellar hematoma, resulting from closed craniocerebral injury. In the first day after thrombolytic therapy, a decrease dyspnea, increase saturation from 74% to 97%, decrease pulmonary artery pressure from 60 to 31 mm Hg, and reduce of right ventricular dysfunction were noted. According to brain CT, on the first day after thrombolysis, an increase in the volume of the subdural hematoma (maximum thickness 8 mm) without dislocation syndrome and without focal neurological deficit was registered. After one week, the patient was discharged. At the follow-up examination after 4 months, regression of the subdural hematoma was noted (the thickness less than 2 mm). The non-immunogenic staphylokinase usage did not lead to major bleeding and hemorrhagic stroke.
Conclusion. The non-immunogenic staphylokinase has shown safety and efficacy in massive PE treatment in an elderly patient with high hemorrhagic risk due to a subdural hematoma.
POINT OF VIEW
Managing a patient with mitral regurgitation (MR) is a difficult task. Degenerative and ischemic changes are the main causes of MR in developed countries, while rheumatic valve changes predominates in developing countries. MR progression occurs gradually and often imperceptibly, which is associated with the compensatory mechanisms of the heart, and leads to left ventricular remodeling and worsens prognosis. The clinical improvement in the patient condition with acute MR after the appearance of heart failure signs is obviously due to a gradual increase in the left atrium and atrial pressure decrease. The initial assessment of MR suggests the presence of heart failure clinical symptoms, which develop as MR volume increases and left ventricular systolic dysfunction worsens. However, these data are insufficient to determine the indications for surgery. Echocardiographic methods should be used to quantify the severity of the defect. The only proven treatment to improve symptoms and prevent heart failure is surgery. The annual mortality rates for surgical treatment in patients aged 50 years and older are about 3% for moderate and 6% for severe MR. Valve-preserving operations are superior in results to prosthetics and reduce mortality in patients with severe organic MR by 70%. The morphology of the valve apparatus lesion is crucial for the successful operation. The consequences of severe rheumatic valve damage limit the possibility of valve repair. If it is impossible to perform valve repair, it is preferable to perform prosthetics of the valve while maintaining the subvalvular apparatus. The best short-term and long-term results of surgical treatment were obtained in asymptomatic patients operated in specialized centers. This highlights the importance of MR early detection and assessment.
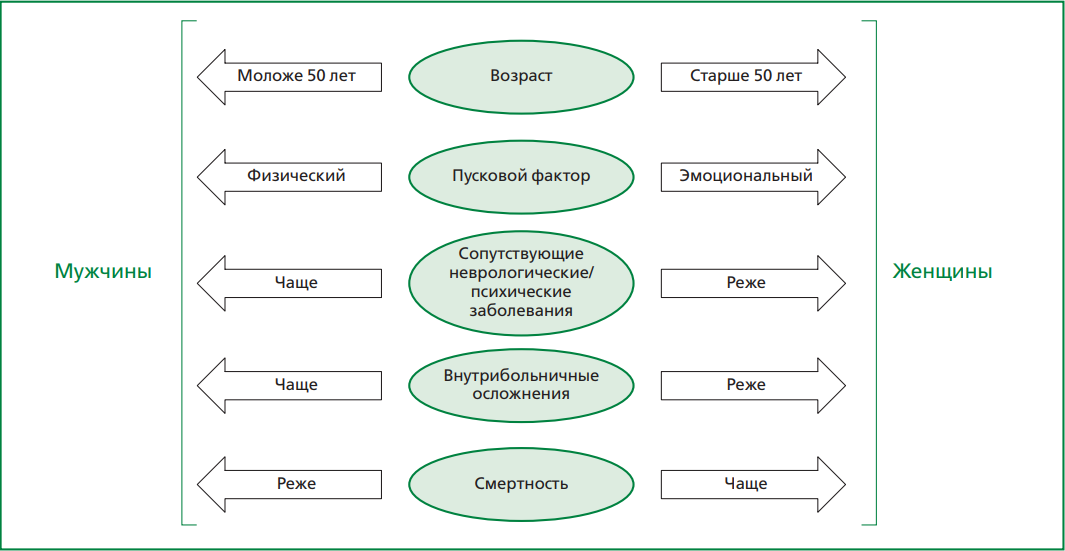
In recent years, there has been increased interest among researchers in the study of Takotsubo syndrome (TS), a special form of reversible left ventricle myocardial dysfunction and, in rare cases, right ventricle dysfunction. It is known that this condition predominantly affects postmenopausal women and is often triggered by physical or emotional stress. However, the pathophysiology of TS remains incompletely understood, with current evidence highlighting the role of catecholamine surge and sympathetic nervous system activation. Given that TS is similar to acute coronary syndrome in terms of clinical and electrocardiographic findings, as well as cardiac biomarker profiles, differential diagnosis between these two conditions is a task enquiring careful clinical judgment. Moreover, despite the reversible nature of TS, it is associated with a high risk of both in-hospital and long-term complications. Echocardiography is the main imaging method to detect the characteristic form of left ventricular akinesia or dyskinesia and to exclude other causes of acute heart failure. Nevertheless, coronary angiography, in which the key sign is the absence of obstructive lesions of coronary arteries, and cardiac magnetic resonance imaging, which assesses myocardial edema, fibrosis, and other structural changes, are of great importance in the TS diagnosis. Thus, a multimodal imagining approach significantly increases diagnostic accuracy and enables timely prognosis assessment in patients. The purpose of this review is to provide up-to-date information on the etiology and clinical features of TS, as well as to discuss current perspectives on its diagnosis.
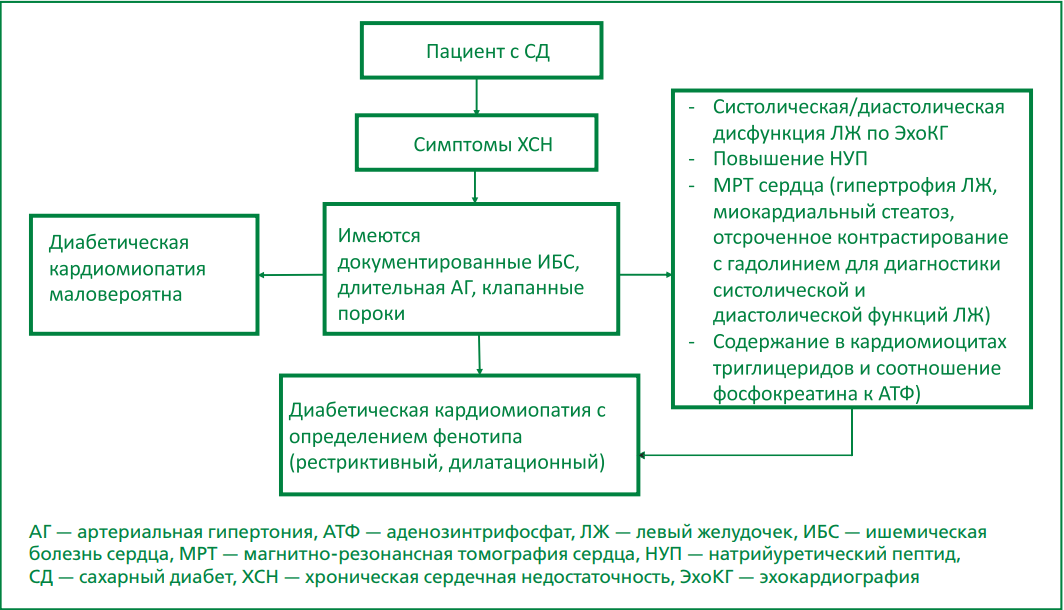
Since the 1970s, researchers have investigated a specific disorder of myocardial structure and function in diabetes mellitus (DM) — diabetic cardiomyopathy (DC) – whose primary clinical manifestation is heart failure (HF). Numerous studies demonstrate a high risk of HF in patients with type 2 diabetes mellitus (T2DM), alongside worsened prognosis when these conditions coexist. For instance, the Kaiser Permanente population study demonstrated a 3- to 4-fold higher HF risk in T2DM patients under 75 years compared to non-diabetic individuals. Despite accumulated research, DCM remains classified by many experts as a complication of DM rather than a distinct entity, fueling ongoing discussion. At the same time, ongoing studies increasingly reveal characteristic disorders of heart function with pathophysiological features, suggesting that DCM may constitute a separate condition occurring within the diabetic context. To date, there are no generally accepted clinical guidelines for DCM diagnosis and management, and therefore there is a need for standardized diagnostic criteria to identify high-risk populations. The review analyzes current literature data on terminology, etiology, pathogenesis, and treatment. Systematisation of existing knowledge and clear diagnostic criteria would facilitate greater focus on novel treatment strategies.
ISSN 2225-3653 (Online)